An Initial Investigation of Neural Changes in Overweight Adults with Food Cravings after Emotional Freedom Techniques
Peta Stapleton 1, * ![]() , Craig Buchan 2
, Craig Buchan 2 ![]() , Ian Mitchell 3
, Ian Mitchell 3 ![]() , Yasmin McGrath 2
, Yasmin McGrath 2 ![]() , Paul Gorton 2
, Paul Gorton 2 ![]() , Brett Carter 1
, Brett Carter 1 ![]()
- School of Psychology, Bond University, Gold Coast, Queensland, 4229, Australia
- Queensland Diagnostic Imaging, Gold Coast, Queensland, Australia
- Siemens Healthcare Pty Ltd, Healthcare Sector, Brisbane, Australia
* Correspondence: Peta Stapleton ![]()
Academic Editor: Gerhard Litscher
Received: December 11, 2018 | Accepted: February 12, 2019 | Published: February 15, 2019
OBM Integrative and Complementary Medicine 2019, Volume 4, Issue 1 doi: 10.21926/obm.icm.1901010
Recommended citation: Stapleton P, Buchan C, Mitchell I, McGrath Y, Gorton P, Carter B. An Initial Investigation of Neural Changes in Overweight Adults with Food Cravings after Emotional Freedom Techniques. OBM Integrative and Complementary Medicine 2019; 4(1): 010; doi:10.21926/obm.icm.1901010.
© 2019 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Background: This pilot randomised clinical trial investigated the effect of Clinical Emotional Freedom Techniques (EFT) on brain activation in response to food craving stimuli using functional magnetic resonance imaging. EFT is a brief stress reduction technique which involves stating a cognitive statement with stimulation of acupressure points with a tapping technique. Method: Fifteen overweight/obese adults were allocated to a four-week group EFT treatment or control condition and completed a measure of food craving. Random repeating images of high-calorie food designed to engage parts of the brain were presented during the pre and post fMRI scans. Results: The Group x Time interaction for food cravings were significant for the EFT group when compared to the controls. Participant mean scores decreased by 18% for the EFT group and 5% for the control group. Brain activity was mapped using fMRI measures, and there was relative deactivation in the Superior Temporal Gyrus and lateral orbito-frontal cortex for the EFT treatment group only. The control group however, showed continued activation in these areas. Conclusion: The findings indicated EFT may decrease limbic region brain activity and reduce food related symptoms in overweight/obese individuals. This study also illuminates the neurological mechanisms at work behind the many successful outcome studies of EFT for weight loss. Recommendations for more comprehensive trials are discussed.
Keywords
Food cravings; overweight; obesity; emotional freedom technique; fMRI; brain
1. Introduction
Obesity is a chronic disease, with an aetiology typically purported to result from a range of causes including metabolic [1], excessive consumption of obesogenic foods [2], genetics [3], environmental contributions that have resulted in more sedentary behaviour such as increased use of transport (e.g. cars), and obesogenic foods being more easily accessible to lower socioeconomic groups because of decreased costs [2]. The likely explanation may well be a combination of these complex, and often interacting processes. What is known is that a five to 10% decrease in body weight for obese adults is associated with significant improvements in blood pressure, serum lipid levels, glucose tolerance [4], and reductions in diabetes [5] and hypertension [6,7]. Existing approaches to addressing the obesity epidemic have included combined dietary and physical activity approaches [8,9] and of late, behavioural or motivation strategies to influence the weight loss process [10,11,12]. Weight loss and weight maintenance, however, are complex issues.
Research suggests dieting regularly results in weight loss in the short term [13] yet, meta-analyses indicate the more time that elapses between the end of a diet and the follow-up period, the more weight is regained [14]. Weight instability has been related to lower health satisfaction and self-esteem and higher body dissatisfaction, dieting, and binge eating [15]. Unfortunately, it is clear that dieting alone does not lead to sustained weight loss and individuals who diet are more likely to gain back more weight than they lost [14].
Adults who are overweight or obese do experience enhanced weight reductions from psychological interventions as well as behavioural approaches [16]. A Cochrane review [16] suggested Cognitive Behaviour Therapy (CBT) and Behaviour Therapy (BT) significantly improved the success of weight loss for overweight and obese adults, but cognitive therapy alone was not found to be effective as a weight loss treatment. The evidence available for other strategies such as relaxation therapy and hypnotherapy also indicated that these might be beneficial in improving weight loss [16].
Energy Psychology (EP) strategies are emerging as techniques which can change emotional, behavioural, and cognitive concerns by combining physical somatic interventions with a cognitive element [17]. Emotional Freedom Techniques (EFT) [18] is one such EP strategy; a type of exposure therapy that includes a somatic and cognitive component for altering the cognitive, behavioural, and neurochemical foundations of psychological problems. Likened to a version of psychological acupuncture, but without the use of fine needles, EFT combines components of traditional approaches (including cognitive and exposure therapy) with acupoint stimulation [18].
Research has found EFT for to be extremely successful and durable over time for treatment of food cravings in overweight and obese adults [19,20,21]. A randomised clinical trial which originally offered a 4-week EFT treatment program to 96 overweight and obese participants with severe food cravings, and then assessed their progress six- and 12-months after treatment ended [19,20] found Body Mass Index (BMI), degree of food craving, individual’s perceived power of food, restraint capabilities and psychological symptoms significantly improved. Weight loss over the 12 months was significant from the start of treatment (mean difference, -5.05 kilograms or 11.1 pounds, p<.05) and the decrease in BMI was also significant (mean difference, -2.28, p<.05; (Stapleton, Sheldon, & Porter, 2012b).
EFT has also been compared to a gold standard therapy. In an overweight/obese sample of adults, EFT and CBT demonstrated comparable efficacy in reducing food cravings, individuals’ responsiveness to food in the environment (power of food), and dietary restraint, with Cohen’s effect size values suggesting moderate to high practical significance for both interventions [22]. Significant decreases in anxiety and depression scores were also reported for subjects in both the EFT and CBT treatment groups, and these benefits were maintained at 12-month follow-up.
These results revealed that EFT was capable of producing treatment effects that were clinically meaningful and comparable to a gold standard approach. Notably, EFT lasted longer over time than CBT for improvements in food cravings and anxious symptomology and subjects’ food cravings, power over food choices, and dieting mentality at the 12-month follow-up [21,22].
For general psychological conditions outside food cravings, several meta analyses have found a very large treatment effect for anxiety (d = 1.23 95% CI: 0.82-1.64, p < 0.001), a very large effect size in the treatment of depression (Cohen's d across all studies was 1.31) [23], and a large treatment effect (weighted Cohen’s d = 2.96, 95% CI 1.96-3.97; p < 0.001) for post-traumatic stress disorder [24]. Research has also indicated treatment gains persist over time [25,26,27,28,29].
Performing the EFT technique while vocalising aspects of a targeted problem (the cognitive element) has been hypothesized to decrease hyperarousal in the amygdala (the stress response area of the brain) and hippocampus (the memory area) [30], alter dopamine and serotonin ratios [17], produce connective tissue transmission of piezoelectric signals [31], and increase HPA axis regulation, which among other benefits reduces stress-related cortisol secretion [32]. Recent research in a sample of veterans with PTSD indicated regulation of six genes associated with inflammation and immunity after 10 EFT sessions, with downregulation of inflammation and stress markers and upregulation of immune markers found [33]. However, despite these studies, it has not been unambiguously established how brain activation and neural mechanisms might be affected by EFT.
1.1 Functional Magnetic Resonance Imaging (fMRI)
Functional Magnetic Resonance Imaging (fMRI) is widely used to map brain activity. fMRI exploits the local increase in blood flow and hence blood volume and blood oxygenation that occur to support the resulting increase in metabolic demand, instead of detecting neuronal activity directly [34]. Brain imaging is a powerful technique that is enhancing neuroscience research. Most conventional fMRI studies are based on the BOLD effect, which is the term used to describe the increase in fMRI signal due to the change in blood oxygenation and blood volume secondary to the increase in blood flow.
Therefore, tracking brain activity with fMRI does not involve direct measurement of neuronal activity. With fMRI, attention is paid to changes in blood flow, blood volume, and blood oxygenation, features of metabolic demand affected by changes in brain activity. Measuring brain activity indirectly is the basic for the BOLD system where changes in brain activity are defined as increases or decreases in blood oxygenation and blood volume secondary to changes in blood flow. Changes in fMRI signal, then, are presumed to be evidence of changes in neural activity.
BOLD fMRI has been used to map the primary cortical representation of taste and odour in humans and to study responses to pleasant and aversive stimuli. Previous neuroimaging studies have shown that emotional distress increases the reward value of palatable food in the brain of restrained eaters [35,36,37]. Studies have also indicated individuals with, versus without substance dependence, show greater activation in brain areas related to reward [38,39] and obese, versus lean adults, show similar activation in response to food cues [40,41].
Due to the emerging evidence indicating EFT can have an immediate and lasting effect on food cravings in obese adults, and given food cravings frequently lead to consumption of the craved food [42], are positively correlated with body mass index (BMI) [39,43] and obese adults report preferences for high fat foods [44], this feasibility study focussed on extending this research further. Subsequently, the study had two objectives:
1. To determine brain activation (using fMRI) in response to high calorie food image stimuli in overweight/obese adults, and 2. To investigate neural mechanisms of symptom improvements in overweight/obese adults following EFT treatment, compared to controls, in order to conduct a larger trial.
2. Materials and Methods
Ethical Approval was provided by the Bond University Human Research Ethics Committee and the trial was registered under the Australia New Zealand Clinical Trials Registry.
2.1 Participants
Ethical Approval was provided by the Bond University Human Research Ethics Committee and the trial was registered under the Australia New Zealand Clinical Trials Registry. The inclusion criteria were: at least 18 years of age, both genders, overweight (i.e. Body Mass Index; BMI; between 25-29) or obese (BMI greater than 30), and not currently receiving treatment (psychological or medical) for their food cravings. Participants who were pregnant, and known sufferers of diabetes (Type I and II) and hypoglycaemia were excluded due to possible craving confound. Because of the fMRI aspect of the study, participants could not have any metal implants (e.g. pace maker) and completed a MRI head safety questionnaire prior to the scan.
After screening, eligible overweight/obese adults were randomly assigned to either the fMRI treatment (N=10) or control group (N=5). All participants completed a pre-survey battery of measures via an electronic link (data not presented here), and underwent a brain scan (fMRI) at a local radiology facility; once for the control group and twice (pre-and post) for the EFT treatment group.
The majority of participants were female (86%), and chocolate was the most commonly chosen food craving to address in the EFT treatment group. The mean age of the EFT group was 48 years and 39 years for the controls; and the average BMI was 37 for the EFT group and 39 for the controls. Results of chi-square analyses revealed there were no significant differences between the EFT and control conditions in baseline sociodemographic characteristics (p>0.05).
2.2 Measures
Anthropometric Measures. Height and weight measurements were obtained to calculate BMI, which is defined as weight in kilograms divided by height in meters squared (kg/m²). BMI categories utilised for the present study included: underweight (< 18.5), healthy weight (18.5 to 24.9), overweight (25.0 to 29.9), or obese (≥ 30.0).
The Food Craving Inventory is a reliable and valid measure for the assessment of cravings for specific types of foods (White et al., 2002). The FCI measures cravings for specific types of foods, namely: High Fats, Sweets, Carbohydrates/Starches, and Fast Food Fats, all of which comprise the higher order construct of “food craving” or the FCI Total score (White & Grilo, 2005). Higher numbers for each of the subscales reflect greater cravings for that food type with the highest score being 185.
2.3 fMRI Paradigm
All participants had an initial (pre) brain scanning session and 5-weeks later at the end of the 4-week EFT intervention. Participants were asked to refrain from eating or drinking prior to the scan (water excepted) and were asked to consume a caffeinated beverage 30-minutes prior (e.g. coffee) to capture the hunger state that most individuals feel prior to their next meal. All scans were completed between 8:00 a.m. and 11:00 a.m., with all participants changed into a gown and presented with safety questions prior to the scan.
The fMRI scans were examined for intracranial structural abnormalities by the Radiologist partner in the study (second author) and the third author interpreted pre-and post-effect differences due to the EFT intervention. During the fMRI scanning the participants were presented with six random repeating images of high-calorie food designed to engage parts of the brain which respond to food stimuli. They were passive during the procedure, except for paying attention to the food images, and this was to minimise engagement of other cognitive systems.
Participants were scanned on a Skyra 3T system on NUMARIS/4 Version Syngo MR E11A, using a 20ch head neck coil combination. A 6:35 mins ep2d_pace_moco sequence was used. This is a single shot Echo planar sequence that has prospective motion correction built within the sequence to correct in real time for motion. In addition, real time monitoring of the amount of motion is possible via the 3D neuro card utilizing the inline features. Block design was used for paradigm creation, and the total number of measurements was 120, with paradigm size being 20 Threshold or T-score was set at 3 for the sequence acquisition. The TR 3200 TE 30 total scan time for sequence was 6:29 minutes, however the use of dummy scans and IPAT calibration accounted for the 6 second disparity. No other filtering was used; synchronization with the scanner ensured that baseline did present until after this period. The Voxel size was 2 x 2 x 3 slices 36 dist factor 0 GRAPPA 2. Block design resulted in baseline, activation, baseline for the duration of test BABA. The paradigm was designed to examine activation in response and anticipated consumption of six food items (see Figure 2). Images were presented via digital projector located outside of the scan room but able to project to a MRI compatible screen. Test subjects were then able to see images via a head mounted mirror.
Activation and baseline periods for the test were 30 seconds. This meant the randomized images were visible for 5.4 seconds each time they were viewed by the subject. When participants saw images, they were advised to imagine tasting and eating each food item as it was presented to them. The duration of each block was designed to be short enough to prevent habituation in the amygdala [45]. In the rest or baseline section a ‘checker board’ image was shown and participates were asked to relax.
Post processing was completed on the scanner using the Neuro 3D platform. Whilst the threshold had been applied on the creation of the paradigm. Final processing of threshold was applied to patient for both data sets to ensure clear visualization of activation area (this gave a threshold of 3.2-4 for all volunteers in cohort). This ensured clarity of data sets for comparison on completion of data collection.
2.4 EFT Treatment
The intervention used in the current trial was ‘Clinical EFT’; the approach has been validated in more than 100 clinical trials. The research supporting Clinical EFT has utilized a protocol which has remained stable through three editions of the EFT Manual [18].
The EFT treatment was offered for two hours per week, for the 4-week period, to the treatment group, while the control group did not engage in any treatment. A trained EFT practitioner counsellor skilled in delivery clinical trials delivered the intervention and all sessions were based on standardised protocols and adhered to the EFT manual [18]. Acupressure points on the eyebrow, side of eye, under eye, under nose, chin, collarbone, under arm, and the top of the head were used.
The procedure of EFT begins by the individual stating a difficulty they are experiencing, followed by an opposing, but positive affirming statement. For example, an individual may state “Even though I am nervous right now, I accept myself and this problem”. Researchers have long found that when positive and negative thoughts are combined, the individual reports a decrease of the negative experience [46]. This combination of positive affirmation and negative thoughts is typically used in Systematic Desensitization, a behaviour modification therapy [46].
Stimulation of specific acupoints then involves tapping on them with two fingers while saying a shorter reminder phrase e.g. “nervous”. The subject rates their level of the problem (nervousness) out of 10 (0 = completely calm, 10 = highest level possible of the issue) before beginning, and re-rates this every time they complete the eight tapping points. The process is repeated until the discomfort score is zero. The EFT treatment sessions involved direct exposure to craved foods with full adherence to protocols and safeguards occurring [18,47]. The group spent two hours using EFT on their food cravings, and were encouraged to self-administer EFT outside of treatment sessions in response to cravings e.g. in the moment of in anticipation). Weekly short message reminders were sent in between sessions to encourage adherence.
3. Results
3.1 Food Craving Analyses
The self-report data was analysed using SPSS (Version 23). An alpha level of .05 was utilised to determine the statistical significance of all results. Inspection of boxplots revealed no extreme outliers.
The test of within subjects effects revealed there was a significant main effect of time for participant total FCI scores, Wilk’s Λ= .485, F (1, 13) = 13.778, p = .003, partial η2= .515. Participant mean scores decreased by 18% for the EFT group (M = 101.1) to post (M = 67.3) and 5% for the control group (M = 83.75 pre; M = 73.25 post). The main effect of group revealed FCI total scores were not significantly different between the EFT (M = 84.300; SE = 3.512) and control (M = 76.400; SE = 4.967) groups, p > .05. The Group x Time interaction for FCI was however significant, revealing the food craving difference scores over time decreased significantly for the EFT group when compared to the controls, Wilk’s Λ= .690, F (1, 13) = 5.830, p = .031, partial η2= .310 (see Table 1).
Table 1 Associated means, standard deviations, and mean differences for the food craving inventory.

3.2 fMRI Analysis
The fMRI scans were analysed as a between-groups whole-brain contrast analysis to identify brain regions activated by anticipation of food. A ‘threshold’ was set to reduce the ‘noisy’ or areas showing activation that were not of interest. Typically with emotive responses the BOLD response is very small so the threshold was set at a level to ensure the areas in question were able to be analysed. The threshold or T-score was set at approximately 2-2.6 (patient dependent). This was then used for all their scans so that comparison could be made with all the tests.
The areas of emotive responses to food and other stimuli have been documented in previous papers and it is noted that there does not appear to be one single area that is definitively identified as the primary response to food. However, in the present study for all the pre-scans, there was relative activation in the superior temporal gyrus (associated with cognition) and lateral orbito-frontal cortex (associated with reward). The post scans for the treatment group only were relatively deactivated in both these areas; there was marked reduction in the BOLD response (see Figure 1 as an example). Post scanning of a control group who did not receive the EFT treatment showed continued activation in these areas (see Figure 2).

Figure 1 Pre and post fMRI for subject in EFT treatment condition.
Note: the yellow, orange and red areas active on the pre scan are relatively deactivated in the post scan of the EFT group.
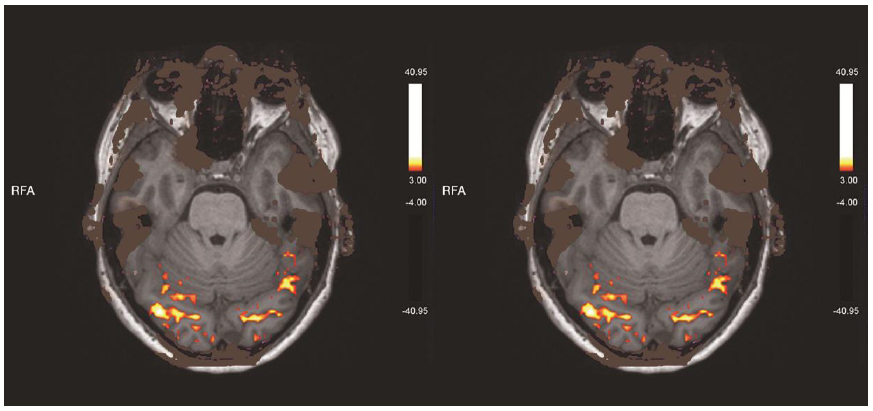
Figure 2 Control group example fMRI scan.
Note: the yellow, orange and red areas active on the pre scan that are still relatively activated in the control group.
4. Discussion
This study represents the first to initially explore neural changes after EFT treatment in overweight/obese adults and was designed to develop a fMRI protocol for future investigations. Our fMRI results were also consistent with those obtained by previous studies and met the first objective. As expected, food images presentation increased activation in the brain and were largest in the superior temporal gyrus and orbitofrontal cortex (left cortical regions). Research suggests even if someone is not hungry, seeing food or thinking about food can stimulate eating [48,49], and cortical regions responsive to food images in previous studies have included the limbic and paralimbic areas [50] and the prefrontal cortex [51].
It has also been noted that while the orbitofrontal cortex is typically associated with reward, it is also activated when non-reward, or loss occurs, and this may be relevant if a subject is imagining being deprived of a food (e.g., a diet or treatment program to target this). The orbitofrontal cortex is the first place where olfactory information and taste information converge [52], therefore, given participants in the present study were explicitly told to imagine eating the food they were viewing, this was not unexpected. Other functional imaging studies have found similar high-calorie items result in more activation than low-calorie control items in the same orbitofrontal cortex region [53,54]. Further, obese participants characteristically show greater neural activation in these brain regions implicated in reward, when compared to lean participants [41,55].
The activation in the superior temporal gyrus in the present study has been noted in other studies. The superior temporal gyrus is significantly activated to a greater extent during the presentation of food items compared to non-food items [56]. Television viewing studies also highlight that food and non-food commercials result in greater activation in neural regions associated with similar attention, focus and language areas [57]. Food images significantly increase activation in healthy controls in this brain area too [58].
The second objective of this study was to compare the EFT treatment group to the controls and ascertain any differences in neural activity after therapy. There were differences between the EFT group on their pre-and post fMRI scans, as well as differences to the control group. The EFT group achieved a marked reduction in activation post their EFT treatment in both the superior temporal gyrus and orbitofrontal cortex, whereas the control group remained the same.
While speculatively, the neural changes indicated in this pilot study appear to compare to the self-reported food craving decreases in the current trial as well as previous EFT and food craving trials [19,20,21,22]. The lack of engagement in homework activities reported by participants (addressed next) and the relative deactivation of the brain activity during the post scans while viewing high caloric food images, suggests a correlation worth examining in larger future trials.
Finally and worthy of note is that while the EFT participants were encouraged to engage in the technique outside sessions, and reminder messages were sent by the lead therapist between sessions every week. However, they typically did not do so via self-report and this was also indicated in previous trials [19,20,21,22]. A recent two year follow-up of an 8-week online intervention program for overweight or obese adults found participants’ food craving, perceived power of food, dietary restraint capabilities and all psychological distress symptoms (i.e. anxiety, depression and somatic) remained significantly reduced from the end of treatment to two-year follow-up [59] with no further treatment and a distinct lack of in-between session homework. This study suggested that using EFT in the sessions alone resulted in a reduction of cravings that did not require any further intervention from the end of the 8-week program.
It is true a common strategy in the gold standard cognitive and behaviour therapies is utilizing homework assignments as a mechanism to produce and strengthen beneficial treatment outcomes. Practicing skills outside the therapy session for permanent and long-term change is essential. Indeed, engaging in homework activities to produce positive therapy outcomes has been examined in meta-analyses and results indicate that greater compliance with homework is associated with more beneficial treatment outcomes [60,61].
However, one of the top cited reasons for therapy failure in CBT is homework noncompliance [62]. In adult clients, the rates of nonadherence range from 20 to 50 percent [63]. As mentioned, EFT’s physical component is more than tapping on the skin (indeed meta-analysis indicates that the acupressure component is an active ingredient and outcomes are not due solely to placebo, nonspecific effects of any therapy, or nonacupressure components [64]). EFT results in changes in the brain, DNA expression, hormone production, brain waves, and blood flow; and is it remarkably swift. This stimulation of acupressure points is indeed a “health promoting activity” that occurs in session, and does not necessarily rely on homework tasks being completed outside this.
It has been suggested that there are three factors common to all successful psychotherapies: the therapist and the client have a strong bond and effective working relationship; the therapist and client both have an expectation that therapy will be successful; and the therapy approach includes the client engaging in health-promoting, beneficial actions [65]. The stimulation of specific acupoints in EFT has been suggested to be this “health promoting activity” and thus does not necessarily rely on homework tasks being completed outside the session [66]. This may answer why the treatment effects last over time, although further research is warranted
4.1 Limitations
This research served as a pilot study for further explorations of brain activation after EFT treatment. Clearly participant numbers were relatively low and restrictive on the inferences that can be drawn. In order to draw direct conclusions future studies should be larger and longer in follow-up periods and individuals perhaps be able to pick the most appropriate food images that they would like to consume at the specific moment of the scan. Subjects in the current study were scanned while fasting; thus, they were hungry during the protocol, which may have enhanced the appeal of high calorie food items. This study examined findings at an individual level because of sample size and to retain individualities in brain structure, however it is recommended that future studies include group brain analyses. Further research may also benefit from investigating the issue of engaging in homework (e.g. further tapping) to ascertain the impact of compliance and longevity of the technique.
4.2 Implications and Future Recommendations
Despite the limitations, this initial study did demonstrate that the viewing of high calorie food items by fasting overweight adults activated brain areas associated with focus and attention (superior temporal gyrus) and reward (orbitofrontal cortex). Furthermore, eight hours of EFT treatment resulted in a relative deactivation of neural activity for those adults and may be a useful adjunct for adults in weight loss and maintenance programs.
Author Contributions
The first author designed and oversaw the clinical trial and wrote the publication with the research assistant sixth author. The second author investigated the fMRI scans for intracranial structural abnormalities and was the Radiologist partner in the study. The third author interpreted pre-and post-effect fMRI scan differences due to the EFT intervention, while the fourth and fifth authors were technical staff present during all scans.
Acknowledgements
This study wishes to acknowledge the EFT practitioner Brett Porter who delivered the intervention for the trial.
Funding
This study acknowledges the private donations of several benefactors (Mrs Pamela Thomas and Alina Frank/Craig Weiner) and Faculty funding from Bond University, as well as the Association of Comprehensive Energy Psychology, USA.
Competing Interests
The first author may derive income from delivering presentations or trainings using the technique investigated in this paper. The remaining authors have declared that no competing interests exist.
References
- Bray GA, DeLany J. Opinions of obesity experts on the causes and treatment of obesity‐A new survey. Obes Res. 2012; 3: 419S-423S. [CrossRef] [Google scholar] [PubMed]
- Wilding J. Are the causes of obesity primarily environmental? Yes. BMJ. 2012; 345. doi: 10.1136/bmj.e5843 [CrossRef] [Google scholar] [PubMed]
- Lyon HN, Hirschhorn JN. Genetics of common forms of obesity: A brief overview. Am J Clin Nutr. 2005; 82: 215S-217S. [CrossRef] [Google scholar] [PubMed]
- Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord. 1992; 16: 397. [Google scholar]
- Colditz GA, Willett WC, Rotnitzky A, Manson JAE. Weight gain as a risk factor for clinical diabetes mellitus in women. Annu Intern Med. 1995; 122: 481. [CrossRef] [Google scholar] [PubMed]
- Huang Z, Willett WC, Manson J, Rosner B, Stampfer MJ, Speizer FE, Colditz GA. Body weight, weight change, and risk for hypertension in women. Annu Intern Med. 1998; 128: 81. [CrossRef] [Google scholar] [PubMed]
- Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005; 13: 876-882. [CrossRef] [Google scholar] [PubMed]
- Fujioka K. Management of obesity as a chronic disease: Nonpharmacologic, pharmacologic, and surgical options. Obes Res. 2012; 10: 116S-123S. [CrossRef] [Google scholar] [PubMed]
- Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001; 21: 323-341. [CrossRef] [Google scholar] [PubMed]
- Bandura, A. The explanatory and predictive scope of self-efficacy theory. J Soc Clin Psychol. 1986; 4: 359-373. [CrossRef] [Google scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. Am Psychol. 1992; 47: 1102. [CrossRef] [Google scholar] [PubMed]
- Prochaska JO, Norcross JC, Fowler JL, Follick MJ, Abrams DB. Attendance and outcome in a work site weight control program: Processes and stages of change as process and predictor variables. Addict Behav. 1992; 17: 35-45. [CrossRef] [Google scholar] [PubMed]
- Perri M, Fuller P. Success and failure in the treatment of obesity: Where do we go from here. Med Exerc Nutr Health. 1995; 4, 255-272. [Google scholar]
- Mann T, Tomiyama AJ, Westling E, Lew AM, Samuels B, Chatman J. Medicare's search for effective obesity treatments: Diets are not the answer. Am Psychol. 2007; 62: 220. [CrossRef] [Google scholar] [PubMed]
- Serdar KL, Mazzeo SE, Mitchell KS, Aggen SH, Kendler KS, Bulik CM. Correlates of weight instability across the lifespan in a population‐based sample. Int J Eat Disorder. 2011; 44: 506-514. [CrossRef] [Google scholar] [PubMed]
- Shaw K, O'Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. 2005: CD003818. [CrossRef] [Google scholar] [PubMed]
- Feinstein D. Energy psychology: A review of the preliminary evidence. Psychother Theory Res Pract Train. 2008; 45: 199. [CrossRef] [Google scholar] [PubMed]
- Church D. The EFT manual. Fulton, CA: Energy Psychology Press; 2014. [Google scholar]
- Stapleton P, Sheldon T, Porter B, Whitty J. A randomised clinical trial of a meridian-based intervention for food cravings with six-month follow-up. Behav Change. 2011; 28: 1. [CrossRef] [Google scholar]
- Stapleton P, Sheldon T, Porter B. Clinical benefits of Emotional Freedom Techniques on food cravings at 12-months follow-up: A randomised controlled trial. Energ Psychol J. 2012; 4: 1-11. [Google scholar]
- Stapleton P, Bannatyne A, Chatwin H, Urzi KC, Porter B, Sheldon T. Secondary psychological outcomes in a controlled trial of Emotional Freedom Techniques and Cognitive Behaviour Therapy in the treatment of food cravings. Complement Ther Clin Pract. 2016; 28: 136-145. [CrossRef] [Google scholar] [PubMed]
- Stapleton P, Bannatyne A, Porter B, Urzi KC, Sheldon T. Food for thought: A randomised controlled trial of Emotional Freedom Techniques and Cognitive Behavioural Therapy in the treatment of food cravings. Appl Psychol Health Well Being. 2016; 8: 232-257. [CrossRef] [Google scholar] [PubMed]
- Nelms J, Castel D. A systematic review and meta-analysis of randomized and non-randomized trials of Emotional Freedom Techniques (EFT) for the treatment of depression. Explore-NY. 2016; 12: 416-426. [CrossRef] [Google scholar] [PubMed]
- Sebastian B, Nelms J. The effectiveness of Emotional Freedom Techniques in the treatment of posttraumatic stress disorder: A meta-analysis. Explore-NY. 2017; 13: 16-25. [CrossRef] [Google scholar] [PubMed]
- Church D. The effect of EFT (Emotional Freedom Techniques) on athletic performance: A randomized controlled blind trial. Open Sport Sci J. 2009; 2: 94–99. [CrossRef] [Google scholar]
- Church D. The treatment of combat trauma in veterans using EFT (Emotional Freedom Techniques): A pilot protocol. Traumatol. 2010 ; 16 : 55-65. [CrossRef] [Google scholar]
- Church D. Your DNA is not your destiny: Behavioral epigenetics and the role of emotions in health. Anti-Aging Med Ther. 2011 ; 13, 35-42. [Google scholar]
- Rowe J. The effects of EFT on long-term psychological symptoms. Counsel Clin Psychol. 2005; 2: 104-111. [Google scholar]
- Wells S, Polglase K, Andrews HB, Carrington P, Baker AH. Evaluation of a meridian-based intervention, Emotional Freedom Techniques (EFT), for reducing specific phobias of small animals. J Clin Psychol 2003 ; 59 : 943–966. [CrossRef] [Google scholar] [PubMed]
- Feinstein D. Rapid treatment of PTSD: Why psychological exposure with acupoint tapping may be effective. Psychother Theory Res Pract Train. 2010; 47: 385-402. [CrossRef] [Google scholar] [PubMed]
- Oschman J. Trauma energetics. J Bodyw Mov Ther. 2006; 10: 21. [CrossRef] [Google scholar]
- Church D. The effect of EFT (Emotional Freedom Techniques) on psychological symptoms: A limited replication. Presented at Science and Consciousness, the Tenth Annual Energy Psychology Conference. 2008; Toronto, Oct 24. [Google scholar]
- Church D, Yount G, Rachlin K, Fox L, Nelms J. Epigenetic effects of PTSD remediation in veterans using Clinical EFT (Emotional Freedom Techniques): A randomized controlled trial. Am J Health Promot. 2016; 32: 112-122. [CrossRef] [Google scholar] [PubMed]
- Macdonald IA, Francis ST, Gowland PA, Hardman CA, Halford JCG. Brain activation in relation to specific dietary components: What does fMRI measure and how should one interpret cravings for certain foods? Am J Clin Nutr. 2013; 98: 633-634. [CrossRef] [Google scholar] [PubMed]
- Cardi V, Leppanen J, Treasure J. The effects of negative and positive mood induction on eating behaviour: A meta-analysis of laboratory studies in the healthy population and eating and weight disorders. Neurosci Biobehav Rev. 2015; 57: 299-309. [CrossRef] [Google scholar] [PubMed]
- Crosby R, Wonderlich, S, Engel, S, Simonich, H, Smyth, J, & Mitchell, J. Daily mood patterns and bulimic behaviors in the natural environment. Behav Res Therapy. 2009; 47, 181-188. [CrossRef] [Google scholar] [PubMed]
- Wagner DD, Boswell, RG, Kelley, WM, & Heatherton, TF. Inducing negative affect increases the reward value of appetizing foods in dieters. J Cognitive Neuroscience. 2012; 24. Doi: 10.1162/jocn_a_00238. http://doi.org/10.1162/jocn_a_00238 [CrossRef] [PubMed]
- McBride D, Barrett SP, Kelly JT, Aw A, Dagher A. Effects of expectancy and abstinence on the neural response to smoking cues in cigarette smokers: An fMRI study. Neuropsychopharmacol. 2006; 31, 2728-2738. [CrossRef] [Google scholar] [PubMed]
- Franken IHA, Muris P. Individual differences in reward sensitivity are related to food craving and relative body weight in healthy women. Appetite. 2005; 45: 198-201. [CrossRef] [Google scholar] [PubMed]
- Stice E, Spoor S, Bohon C, Veldhuizen M, Small D. Relation of reward from food intake and anticipated food intake to obesity: A functional magnetic resonance imaging study. J Abnorm Psychol. 2008; 117: 924-935. [CrossRef] [Google scholar] [PubMed]
- Stoeckel LE, Weller RE, Cook E, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. NeuroImage. 2008; 41: 636-647. [CrossRef] [Google scholar] [PubMed]
- Hill AJ, Heaton-Brown L. The experience of food craving: A prospective investigation in healthy women. J Psychosom Res. 1994; 38: 801-814. [CrossRef] [Google scholar] [PubMed]
- Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioural correlates of baseline BMI in the Diabetes Prevention Program (DPP). Diabetes Care. 2002; 25, 192-198. [CrossRef] [Google scholar] [PubMed]
- Drewnowski A, Kurth C, Holden-Wiltse J, Saari J. Food preferences in human obesity: Carbohydrates versus fats. Appetite. 1992; 18: 207-221. [CrossRef] [Google scholar] [PubMed]
- Haas BW, Constable RT, Canli T. Functional magnetic resonance imaging of temporally distinct responses to emotional facial expressions. Soc Neurosci. 2009; 4: 121-134. [CrossRef] [Google scholar] [PubMed]
- Kazdin AE, Wilcoxon LA. Systematic desensitization and nonspecific treatment effects: A methodological evaluation. Psychol Bull. 1976; 83: 729-758. [CrossRef] [Google scholar]
- Flint GA, Lammers W, Mitnick DG. Emotional freedom techniques. J Aggress Maltreat T. 2005; 12: 125-150. [CrossRef] [Google scholar]
- Berthoud HR. The neurobiology of food intake in an obesogenic environment. Proc Nutr Soc. 2012; 71: 478-487. [CrossRef] [Google scholar] [PubMed]
- Smeets PA, Erkner A, de Graaf C. Cephalic phase responses and appetite. Nutr Rev. 2010; 68: 643-655. [CrossRef] [Google scholar] [PubMed]
- Tataranni PA, et al. Neuroanatomical correlates of hunger and satiation in humans using positron emission tomography. P Nat Acad Sci. 1999; 96, 4569-4574. [CrossRef] [Google scholar] [PubMed]
- Ioannou S, Williams AL. Preliminary fMRI findings concerning the influence of 5‐HTP on food selection. Brain Behav. 2017; 7: e00594. [CrossRef] [Google scholar] [PubMed]
- Rolls ET, Deco G. Non-reward neural mechanisms in the orbitofrontal cortex. Cortex. 2016; 83: 27-38. [CrossRef] [Google scholar] [PubMed]
- Goldstone AP, et al. Fasting biases brain reward systems towards high-calorie foods. Eur J Neurosci. 2009; 30: 1625-1635. [CrossRef] [Google scholar] [PubMed]
- Killgore WDS, Young AD, Femia LA, Bogorodzki P, Rogowska J, Yurgelun-Todd DA. Cortical and limbic activation during viewing of high- versus low-calorie foods. Neuroimage. 2003; 19: 1381-1394. [CrossRef] [Google scholar] [PubMed]
- Martin LE, et al. Neural mechanisms associated with food motivation in obese and healthy weight adults. Obesity. 2009; 18: 254-60. [CrossRef] [Google scholar] [PubMed]
- St-Onge MP, Sy M, Heymsfield SB, Hirsch J. Human cortical specialization for food: A functional magnetic resonance imaging investigation. J Nutr. 2005; 135: 1014-1018. [CrossRef] [Google scholar] [PubMed]
- Buchsbaum BR, Hickok G, Humphries C. Role of left posterior superior temporal gyrus in phonological processing for speech perception and production. Cogn Sci. 2001; 25: 663-678. [CrossRef] [Google scholar]
- Brooks SJ, O′Daly OG, Uher R, Friederich HC, Giampietro V, Brammer M, et al. Differential neural responses to food images in women with Bulimia versus Anorexia Nervosa. PLoS One. 2011; 6: e22259. [CrossRef] [Google scholar] [PubMed]
- Stapleton P, Lilley-Hale ES, Mackintosh G, Sparenburg E. Online delivery of Emotional Freedom Techniques for food cravings and weight management: Two year-follow-up. J Altern Complement Med. 2019, under review. [Google scholar]
- Kazantzis N, Deane FP, Ronan, KR Homework assignments in cognitive and behavioral therapy: A meta-analysis. Clin Psychol-Sci Pr. 2000; 7: 189-202. [CrossRef] [Google scholar]
- Mausbach BT, et al. The relationship between homework compliance and therapy outcomes: An updated meta-analysis. Cogn Ther Res. 2010; 34: 429-438. [CrossRef] [Google scholar] [PubMed]
- Helbig S, Fehm L. Problems with homework in CBT: Rare exception or rather frequent? Behav Cogn Psychoth. 2004; 32: 291-301. [CrossRef] [Google scholar]
- Kazantzis N, Lampropoulo GK, Deane FP. A national survey of practicing psychologists’ use and attitudes toward homework in psychotherapy. J Consult Clin Psychol. 2005; 73: 742-748. [CrossRef] [Google scholar] [PubMed]
- Church D, Stapleton P, Yang A, Gallo F. Is Tapping on acupuncture points an active ingredient in emotional freedom techniques? A systematic review and meta-analysis of comparative studies. J Nerv Ment Dis. 2018; 206: 783-793. [CrossRef] [Google scholar] [PubMed]
- Wampold B. How important are the common factors in psychotherapy? An update. World Psychiatry 14, no3; 2015; 270-277. doi:10.1002/wps.20238. [CrossRef] [Google scholar] [PubMed]
- Stapleton P. The science behind tapping. Hay House: California; 2019. [Google scholar]


