The Efficacy of Mindfulness-Based Interventions on Depressive Symptoms and Quality of Life: A Systematic Review of Randomized Controlled Trials
Jonathan Manh Dang, MD 1 ![]() , Luma Bashmi, MA 1
, Luma Bashmi, MA 1 ![]() , Stephen Meeneghan, ND, LAc 3
, Stephen Meeneghan, ND, LAc 3 ![]() , Janet White, MD 3
, Janet White, MD 3 ![]() , Rebecca Hedrick, MD 1
, Rebecca Hedrick, MD 1 ![]() , Jelena Djurovic, MA 6
, Jelena Djurovic, MA 6 ![]() , Brigitte Vanle, PhD 1
, Brigitte Vanle, PhD 1 ![]() , Dennis Nguyen, DO 5
, Dennis Nguyen, DO 5 ![]() , Jonathan Almendarez, BA 1
, Jonathan Almendarez, BA 1 ![]() , Paula Ravets, PhD 4
, Paula Ravets, PhD 4 ![]() , Yasmine Gohar, BA 1
, Yasmine Gohar, BA 1 ![]() , Sophia Hanna, BA 1
, Sophia Hanna, BA 1 ![]() , Itai Danovitch, MD 1
, Itai Danovitch, MD 1 ![]() , Waguih William IsHak, MD, FAPA 1,2,*
, Waguih William IsHak, MD, FAPA 1,2,* ![]()
- Department of Psychiatry and Behavioral Neurosciences, Cedars-Sinai Medical Center, Los Angeles, California, USA
- Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California, USA
- Department of Integrative Health, Cedars-Sinai Medical Center, Los Angeles, California, USA
- Department of Spiritual Care, Cedars-Sinai Medical Center, Los Angeles, California, USA
- Kansas City University of Medicine and Biosciences, Rockhurst University Helzberg School of Management, Kansas, Missouri, USA
- Illinois School of Professional Psychology at Argosy University, Schaumburg, USA
* Correspondence: Waguih William IsHak, M.D., FAPA ![]()
Received: March 28, 2018 | Accepted: June 15, 2018 | Published: June 25, 2018
OBM Integrative and Complementary Medicine 2018, Volume 3, Issue 2 doi:10.21926/obm.icm.1802011
Academic Editor: Sok Cheon Pak
Special Issue: Health Benefits of Meditation
Recommended citation: Dang JM, Bashmi L, Meeneghan S, White J, Hedrick R, Djurovic J, Vanle B, Nguyen D, Almendarez J, Ravets P, Gohar Y, Hanna S, Danovitch I, IsHak WW. The Efficacy of Mindfulness-Based Interventions on Depressive Symptoms and Quality of Life: A Systematic Review of Randomized Controlled Trials. OBM Integrative and Complementary Medicine 2018;3(2):011; doi:10.21926/obm.icm.1802011.
© 2018 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Background: An increasing number of patients and practitioners are using mindfulness meditation programs despite uncertainty about the evidence supporting these programs’ health benefits. Aim: To review the current evidence on the effectiveness of mindfulness-based interventions (MBI) on depressive symptoms and quality of life (QOL) among patients with depression comorbid medical conditions and those with major depressive disorder. Methods: A comprehensive search of PubMed, Ovid MEDLINE, and PsycINFO was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the past 30 years (1987-2017) published in English. The following keywords were used: meditation, QOL, depression, and mindfulness. Based on the consensus of two reviewers, 16 studies were selected for inclusion in this study. Results: We included randomized controlled trials that utilized mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT) and other programs that based on MBSR and MBCT protocols. Overall, these interventions showed significant improvement in depressive symptoms and Quality of Life (QOL) at posttreatment (8 weeks) compared to usual care, waitlist-control, active control (psycho-education, exercise, and muscle relaxation), and evidence-based treatment (antidepressants). The interventions were found to be useful, especially among patients with depression dealing with chronic pain, cancer, multiple sclerosis, amyotrophic lateral sclerosis, irritable bowel syndrome, and insomnia. Conclusions: MBSR, MBCT, and mindfulness interventions that modeled MBSR/MBCT appear efficacious as a treatment for depressive symptoms (alone and adjunctive therapy) among patients suffering from depression comorbid medical conditions, and those with major depressive disorder.
Keywords
Depression; quality of life; mindfulness; meditation
1. Introduction
Depression, including major depressive disorder, is a common illness worldwide, with more than 300 million people affected. [1] Current predictions indicate that by 2030, depression will be the leading cause of disease burden globally. [2] The impact of depression extends beyond symptom severity, as depression has a significant impact on quality of life (QOL). [3,4] The World Health Organization describes QOL as the subjective evaluation of life domains including physical health, psychological state, personal belief, and social relations, all within an individual’s respective environmental and cultural context. [5] Depression is commonly treated with antidepressants or psychotherapy, or a combination of both. Both can be effective in reducing the symptoms of depression5, but studies consistently show low remission rates and high dropout rates for these therapies. [6,7,8,9] Furthermore, in patients with comorbid medical illness, pharmacotherapy for depression carries a risk for increased side effects and drug-drug interactions. [10] In view of the debilitating impact of depression, there is a need for new depression treatments with a more favorable risk/benefit profile. Currently, there is a strong interest in utilizing complementary and alternative therapies for depression and other psychiatric disorders among both patients and practitioners. [11,12] For example, psychotherapy experts predict that “mindfulness” meditation will be the most common therapeutic orientation utilized over the next ten years. [13]
Meditation is defined as a practice that involves mental training and regulating attention to achieve well-being and emotional balance. [14] Meditation encompasses a family of complex practices that include mindfulness meditation, mantra meditation, yoga, Tai Chi, and Qi Gong. [15] The word mindfulness derives from the Pali word sati, which means, “to remember”. [16] One of the first modern definitions of mindfulness was described by Jon Kabat-Zinn as the ability to maintain open, accepting, and nonjudgmental awareness in the present moment. [17] The practice of mindfulness meditation refers to a particular kind of attention characterized by a nonjudgmental awareness of present thoughts, emotions, and body sensations, simply observing them as they arise and pass away rather than acting on them impulsively. [18,19] In recent years, growing attention has been given to mindfulness meditation and mindfulness-based interventions (MBI) in the management of health conditions. [20,21,22,23,24,25,26,27] Despite the growing popularity and the various benefits of meditation, there is still skepticism from the clinical science field, as its effects on depression and QOL have not been adequately established.
Many reviews have been conducted to examine the efficacy of MBI on depression. [20,28,29,30,31,32,33] These reviews generally reported that MBI may have mild to moderate effectiveness in reducing depressive symptoms. However, most of these reviews do not define “mindfulness” in a systematic way [34]; instead, it is used as an umbrella term to cover: Vipassana meditation [35], Zen meditation [36], Mindfulness-Based Stress Reduction (MBSR) [37], Mindfulness-Based Cognitive Therapy (MBCT) [38], Acceptance and Commitment Therapy [39], Dialectical Behavior Therapy [40], mindfulness training based on MBSR and MBCT, [41,42] and Transcendental Meditation. [43] Furthermore, existing reviews demonstrate inconsistent findings. On one hand, a recent meta-analysis [28] examining the effect of MBI on depression concluded that at post-treatment, MBI were superior to specific active controls (exercise, drugs, psycho-education, and other therapies). On the other hand, Goyal et al [29] reported no differences between mindfulness meditation programs and specific active controls. Other studies examined the effects of MBI on mood symptoms also came to divergent conclusions. A study conducted by Toneatto and Nguyen [44] suggested that MBI had no reliable effect in treating mood disorders. In contrast, Baer reported that MBI may be helpful for these disorders. [20] The current paper focuses on depression and QOL as clinical outcomes since depression has a substantial risk of recurrence and a significant impact on QOL.
The present study aims to provide a comprehensive review of the two most commonly used interventions (MBSR [37], MBCT [38]) among the MBI and to review the current evidence of its effectiveness on depressive symptoms and QOL among adult patients suffering from depression comorbid medical illness and those with major depressive disorder.
Ethics Statement
Ethical approval is not required as the current study does not include confidential participant data and interventions. This study only extracts and synthesizes data from previous clinical trials in which informed consent has already been obtained by the trial investigators. The current study is addressing very similar questions to the research question from which the data were collected.
2. Materials and Methods
2.1 Literature search
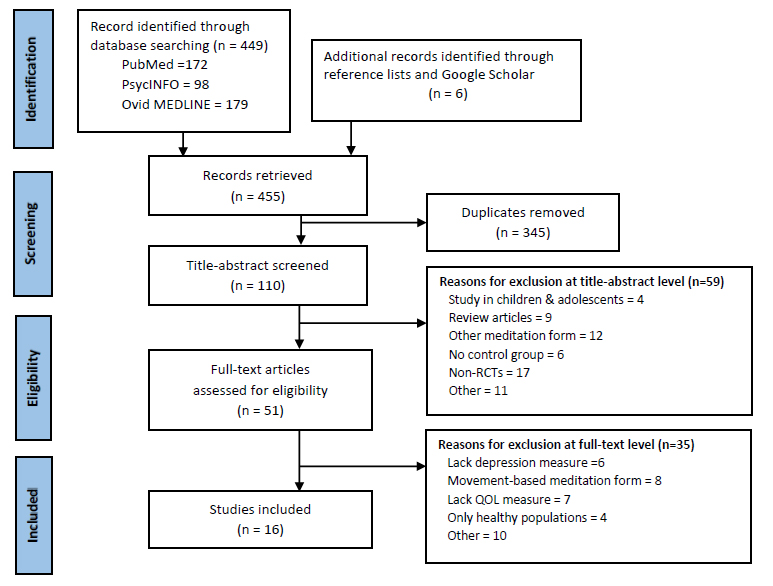
Figure 1 PRISMA* Flow diagram for systematic review detailing study selection.
*PRISMA (Preferred Reporting Items for Systematic Reviews & Meta-Analyses) described in Moher et al. [45]
A systematic literature search was conducted using PubMed, OVID MEDLINE, and PsycINFO databases for articles published over the past 30 years (1987-2017). Each database was searched using the following keywords: “Depress*” AND “meditation” AND “quality of life”, “QOL,” AND “mindfulness.” We reviewed the reference lists of the retrieved articles and relevant systematic reviews to identify articles missed in the database searches. The initial search identifies 455 articles: 345 were eliminated because they were duplicates and 110 were then screened based on the selection criteria (Figure 1).
2.2 Study selection criteria
Two reviewers (JD and WI) independently evaluated the titles and abstracts of the 110 retrieved articles to determine if they met eligibility criteria. The inclusion criteria were: (1) Adults aged 18 years or older, (2) Medical or psychiatric diagnosis, (3) MBSR, MBCT, and mindfulness-based programs that modeled MBSR or MBCT, (4) English language, (5) Randomized-controlled trials (RCTs), (6) Studies that focused on the following outcome measures: depression, meditation, and QOL. Exclusion criteria were: (1) Studies conducted in children or adolescents, (2) Studies of only healthy individuals, (3) Transcendental Meditation, Zen meditation, Vipassana meditation, movement-based meditations (such as yoga, tai chi, and qi gong), hypnosis, breathing exercises (pranayama), and any interventions that did not involve the physical presence of a meditation teacher (surveys, video, audio, or internet meditations), (4) Review articles, (5) Non-RCTs, and case studies, (6) Studies that did not address symptoms of depression and QOL as primary or secondary outcome measures.
The reason for including populations with medical or psychiatric diagnoses is to examine the effectiveness of mindfulness meditation on a broader range of populations and depressive symptom severity. We included MBSR and MBCT because these have established protocols and are commonly used interventions among the MBI. For the purpose of quality, we only included RCTs. We limited our study to adults and those in English publications to avoid misinterpretation of data due to translation. We excluded Dialectical Behavioral Therapy and Acceptance and Commitment Therapy because therapists guiding the interventions are not necessarily trained meditation teachers or had received supervision from trained meditation teachers.
Both reviewers (JD, WI) then independently conducted a focused review using the full text articles of studies that met the above criteria. Following this, the reviewers reached a consensus about the studies to include in this manuscript. The study selection process yielded 16 articles shown in Figure 1. The list of all the 35 excluded articles with their reasons of exclusion will be provided upon request.
2.3 Data extraction
Two reviewers (JD, WI) extracted information on general study characteristics, interventions, effect sizes, p-values, means/standard deviations, main findings, and outcome measures such as depression and QOL. For each meditation program, we extracted information on the type of meditation, hours of training, study duration and follow-up, amount of home practice, and control groups (waitlist, treatment as usual, active control, evidence-based treatment). We resolved differences between investigators regarding data through consensus.
2.4 Risk of bias and study quality
The quality of each article was assessed using the Cochrane risk of bias tool. [46] The Cochrane tool includes six criteria against which potential risk of bias is judged: Random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selectivity of outcome reporting, and other biases. A summary of the risk of bias is presented in Table 2. The quality of the included studies was rated by LB and JD. Any discrepancies were discussed and resolved. For the present study, an AMSTAR 2 checklist (Table 3) was used to ensure all items of a good quality systematic review were addressed. AMSTAR 2 consists of 16 items in total; each item allows for the following response options: Yes, Partial Yes, or No. AMSTAR 2 is not intended to be scored.
Table 1 Characteristics of Included studies.

Table 2 Risk of bias for included studies assessed by Cochrane Risk of Bias Tool.

Table 3 AMSTAR Checklist. [63]

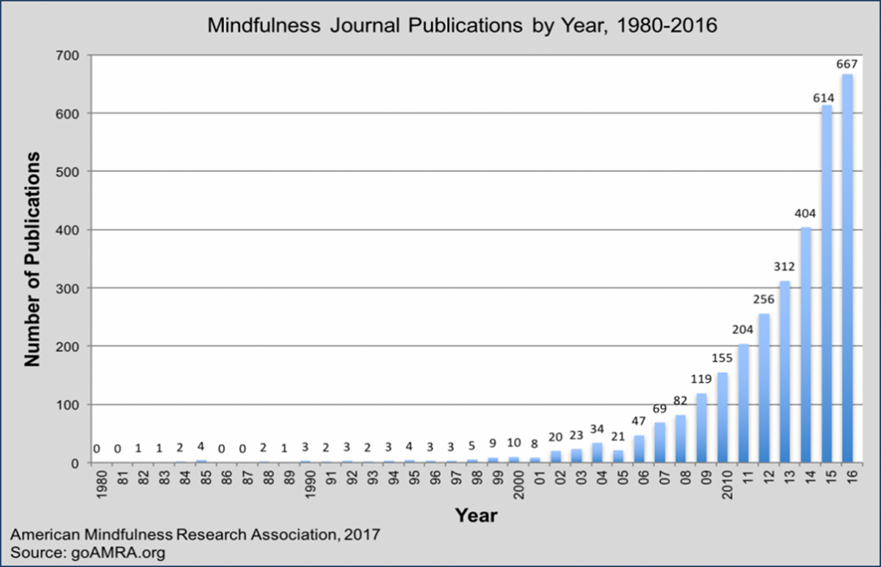
Figure 2 Scientific research into mindfulness.
3. Results
3.1 Description of included studies
We identified 455 citations through searches of electronic databases. Full texts were obtained for 51 citations identified as potentially eligible by two independent reviewers; 16 randomized control trials [47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62] met inclusion criteria (Table 1). Increasing interest in the potential benefits of mindfulness is demonstrated in the rapid rise in published data on the subject. While the literature search for our systematic review looked for publications as far back as 30 years, it is interesting to note that studies that met the criteria (16 studies in total) were found only within the past 16 years (Figure 2). In total, studies assigned 1,536 participants and sample sizes ranged from 16 to 168.
3.1.1 Type of intervention and comparison group
Five studies were conducted using MBSR, five using MBCT, and six using modified MBSR. Eight studies compared MBI to active control (e.g. psycho-education, aerobic exercise/relaxation, health/nutrition education), [49,50,51,52,54,56,59,62] two compared MBI to medications (Eszopiclone, antidepressants), [55,61] and six compared MBI to treatment as usual or waitlist control. [47,48,53,57,58,60]
Eleven studies used MBSR as monotherapy [47,48,50,51,53,54,55,56,57,58,59,62] in depressed patients with comorbid medical conditions and five utilized MBCT as an adjunctive therapy in major/recurrent depression without comorbid conditions. [49,52,57,60,61]
3.1.2 Medical/Psychiatric diagnoses of populations
Eleven studies examining depressed population with comorbid conditions (Amyotrophic Lateral Sclerosis, Chronic Pain, Multiple Sclerosis, Breast Cancer, Irritable Bowel Syndrome, Fibromyalgia, Transplantation, and Chronic Insomnia) utilized MBSR as an intervention. Five studies examining depression without comorbidity utilized MBCT as an intervention. [49,52,57,60,61] One study looked at emotional distress (not specified) and one looked at generalized social anxiety disorder.
3.1.3 Duration, frequency, and follow-up of interventions
The total length of the interventions ranged from 7 to 8 weeks; the majority of interventions (15 studies) were 8 weeks in length. On average, participants were asked to commit to the activities required by their program once a week for 2.5-hours per session. Additionally, a daily 40-45-min mindfulness practice (meditation/exercise) at home was required in 14 studies. Thirteen studies incorporated up to three months follow-up with their participants, occurring at 3 and 6-months after baseline measures were collected (range: 1-24 months).
3.1.4 QOL measures
The majority of the studies measured QOL as a primary or secondary outcome with the exception of one study, which measured depression but not QOL. [60] There were a variety of measures used to assess QOL: the Amyotrophic Lateral Sclerosis Specific QOL Instrument-Revised (ALSSQOL-R), 36-item Short Form Health Survey (SF-36), 12-item Short Form Health Survey (SF-12), the Psychological General Well-Being Index (PGWBI), Functional Assessment of Cancer Therapy-Breast (FACT-B), Satisfaction With Life Scale (SWLS), Irritable Bowel Syndrome QOL (IBS-QOL) questionnaire, QOL Profile for the Chronically Ill Scale (PLC), QOL in Depression Scale (QLDS), Profile of Health-Related QOL in Chronic Disorders (PQOLC), Visual Analogue Scale for QOL (QOL-VAS), and World Health Organization QOL Assessment-Brief (WHOQOL-BREF). The most common measures were the SF-36 and SF-12, which were in three studies each. [48,54,55,59,62] The majority of the QOL measures were multidimensional (a minimum of two and maximum of eight domains) with the exception of the SWLS and QOL-VAS (both unidimensional). The multidimensional measures overlapped in several domains with the majority including the following domains: physical symptoms/functioning, emotional well-being, general health, mental/psychological health, social relationships, and vitality. This demonstrated that QOL was being measured similarly in the majority of studies in this review. All measures were subjective and relied on patient self-reporting. The SF-36, SF-12, PGWBI, and WHOQOL-BREF provided a global assessment of health-related QOL, whereas ALSSQOL-R, FACT-B, IBS-QOL, PLC, QLDS, QOL-VAS, and PQOLC were disease specific. These measures had additional questions or domains that were specific to the disease (e.g., IBS-QOL included two domains not found in other QOL measures in this review: body image and food avoidance). While not all QOL measures were identical in how they measured QOL, they all covered similar components of QOL, providing high reliability and validity coefficients.
3.1.5 Risk of bias and study quality
The quality of each article was assessed using the Cochrane risk of bias tool. Although the potential bias was low across all studies, due to the nature of the type of interventions, most studies were at risk for performance bias with participants clearly aware of their group allocation (Table 2). The overall quality of the included studies is considered high with most studies having low risk of bias across most items. Furthermore, there are no critical weaknesses among the included studies and most provide an accurate summary of the results.
3.2 Efficacy of MBI on depression and QOL
Overall, MBI, specifically MBSR and MBCT, significantly improved depressive symptoms and QOL compared to treatment as usual, waitlist control, active control, and evidence-based treatment among patients suffering from depression with comorbid medical conditions. These benefits were demonstrated in a relatively short amount of time (ranging from 8 weeks to 6 months), which is similar to the amount of time that it often takes to see maximum benefit from pharmacological therapy. [64]
We identified 8 RCTs comparing MBI to active control. Two studies that compared the effectiveness of MBSR to exercise control reported significant improvement in depressive symptoms and QOL. [51,56] For example, Jazaieri et al [51] demonstrated that MBSR and aerobic exercise were effective in improving depression and QOL post-treatment and at 3 months follow-up among patients with social anxiety disorder, but the difference between the interventions was not statistically significant (p=0.53). However, Schmidt and colleagues [56] found that MBSR was superior to exercise (active control) among females with fibromyalgia (within group analysis: MBSR group baseline Mean=25.19 vs post-treatment Mean=23.20, at 2-month f/u Mean=21.70, p=0.012, effect size-ES=0.36; Exercise group baseline M=22.92 vs post-treatment M=20.90, at 2-month f/u M=22.25, p=0.79, ES=0.04). While patients in the MBSR group appeared to benefit the most, the effect sizes were small and did not reflect a statistically significant difference between the two interventions.
Two studies comparing the effectiveness of MBI [49,52] in patients with major depression reported a significantly higher improvement in QOL and depressive symptoms in the MBCT group compared to the psycho-education group. Only one study did not report any improvement in depression. [54] Wong and colleagues’ study [54] examined the effectiveness of MBSR compared to a multidisciplinary pain intervention in treating chronic pain. The study demonstrated that both interventions were effective at improving pain intensity but did not show significant improvement in depressive symptoms and QOL. In another study by Henderson et al., [50] MBI also demonstrated a greater improvement in depression and QOL compared to the nutrition education control group in female patients dealing with breast cancer. Interestingly, a study conducted by Moritz et al [62] reported a greater improvement in depressive symptoms (p=.034) and QOL (p=0.29) in a spirituality group compared to the MBSR group at the end of the 8-wk intervention.
MBI were shown to be superior than treatment as usual (TAU) or wait list control in 6 RCTs. [47,48,53,57,58,60] MBSR was associated with greater improvement in depressive scores and QOL measures compared to TAU in 4 studies [47,48,53,58] among patients with depression comorbid medical conditions. MBCT showed significantly fewer relapse compared to TAU in 2 studies [57,60] in patients with major depressive disorders. For example, a study conducted by La Cour et al [48] concluded that MBSR showed greater improvement on depression (Cohen’s d=.37, p=0.05) and QOL (Cohen’s d=.39, p=0.04) compared to waitlist control at the end of the 8-wk intervention. A recent study [47] comparing MBSR to usual care control among depressed patients with Amyotrophic Lateral Sclerosis demonstrated significant improvement in depression and QOL (p=0.015, d=0.89) in both groups, with greater improvement in depression in the MBSR group. In another study, Godfrin et al [57] reported that MBCT TAU showed significantly fewer relapse than TAU alone (N=12/40 vs N=32/47, p < 0.0005). Adding MBCT to TAU significantly improved QOL.
MBI were also shown to be superior to antidepressants in terms of improving residual depressive symptoms and comparable to antidepressants in terms of relapse prevention. For example, a study conducted by Kuyken et al. [61] in patients with three or more previous episodes of depression and currently symptomatic concluded that MBCT was more effective than antidepressants in improving QOL and reducing residual depressive symptoms as measured by the Beck Depression Inventory (BDI-II; MBCT group baseline Mean=18.51, at 1-month post-treatment Mean=13.12, at 15 months follow-up Mean=12.61; Antidepressant group baseline Mean=20.15, at 1-month post-treatment Mean=17.47, at 15 months follow-up, Mean=17.02). The study randomized 62 patients to traditional antidepressant and 61 to MBCT plus taper/discontinue antidepressant. Relapse rates over a 15-month follow up were 47% in the MBCT group compared to 60% in the antidepressant group. In addition, 75% of the patients in the MBCT group completely discontinued their antidepressants.
4. Discussion
The aim of this study was to review current evidence on the effectiveness of MBI, specifically MBSR, MBCT, and modified MBSR on depressive symptoms and QOL. MBI were shown, in general, to be superior to treatment as usual, waitlist, and active control conditions at the end of the 8-week intervention and follow-up (up to 6 months) among patients suffering from depression with and without comorbid illnesses. This finding is consistent with several meta-analysis reviews. [28,31,32,33] Compared to other evidence-based treatments (e.g. antidepressants), MBCT was more effective than antidepressants in reducing residual depressive symptoms as shown in Kuyken et al. [61]
Our findings demonstrated a significant improvement in QOL in patients suffering from various health problems following an 8-week training in a mindfulness program. A recent RCT [48] examining the effects of mindfulness meditation among individuals with chronic pain found evidence of improvement in health-related QOL and wellbeing compared to wait list control (Cohen’s d=.39, p=0.04). It also suggested that the results may have treatment implications for other chronic conditions that diminish health-related QOL. Results from other carefully performed trials that did not comply with our selection criteria also point to the efficacy of MBI on QOL. [65,66,67] For example, a prospective observational study [68] examining the efficacy of MBSR on QOL among a heterogeneous population reported that health related QOL was enhanced as demonstrated by improvement on all indices of the Short-Form-36 (p<0.01).
One possible explanation for this wide-reaching benefit is how mindfulness works on a psychological level. Depression often results in feelings of fear, negative beliefs, and ruminating thoughts about one’s situation and negative feelings about oneself. The act of mindfulness enables one to develop a different approach to difficult experiences. It empowers the practitioner with the ability to be aware of these thoughts, feelings, and beliefs as they arise and then allows one to observe and/or engage in them in a compassionate and non-judgmental way. [69] These qualities are cultivated as the practitioner spends time each day in a period of silence focusing on the present moment experience, and then carries the moment to moment awareness in to various aspects of daily living. Mindfulness research has identified benefits such as reduced rumination, less emotional reactivity, and enhanced self-insight and fear modulation. A second explanation is that mindfulness helps patients develop a feeling of empowerment by actively participating in a therapeutic intervention. This can stimulate internal locus of control, increase feelings of self-efficacy and the ability to have some control over their experiences. [70]
Depression is one of the main hurdles in medical recovery, often leading to a longer and slower recovery process. A reduction in depression can decrease the recovery time and increase the quality of the recovery process. [71] Hence, reducing depression and improving emotional well-being are one of the crucial goals of the recovery process. In the studies included in this review we found that MBSR, MBCT, and modified MBSR are effective in reducing depressive symptoms and improving QOL.
4.1 Research limitations/strengths
Previous reviews of mindfulness meditation have discussed the challenges posed by this body of research. These include researcher biases (e.g., many researchers are also meditators), confounding variables such as changes in lifestyle and diet that might accompany the meditation practice, and lower methodological quality of research studies as reflected in small sample sizes, limited number of controlled longitudinal studies, and the need for study replication. Another confound that may lend to weak effect sizes is gender. For example, while these therapeutic techniques appear to be effective in women, one study did not find any significant improvement in men with prostate cancer when they were in an MBCT program. [72] This gender difference might be due to differences in the thought processes and attitudes towards meditation-based techniques and/or perception of pain (i.e., specifically, higher subjective appraisal of pain severity amongst women) by the two sexes. [73] Future studies need to address gender differences before implementing these techniques in clinical settings. A major strength of this review is the use of high quality randomized control trials with active controls that controlled for placebo effects (e.g., attention and expectations) as seen in trials using a wait-list or usual care control.
5. Conclusion
MBI are potentially beneficial to people with depression with or without comorbid conditions. Our current review demonstrated that MBI, especially MBSR alone, significantly reduces depressive symptoms and improves QOL among patients suffering from mild depression in addition to other medical illnesses. MBCT incorporated as an adjunctive therapy significantly reduced residual depressive symptoms in patients with major depression.
Acknowledgements
Data used in the preparation of this article were obtained from MEDLINE/PubMed databases. The primary purpose of this research study was to determine the impact of mindfulness-based interventions on depression and quality of life.
Author Contributions
This work was carried out in collaboration between all authors. JMD, WWI, LB, SM, JW, RH, JD, and BV wrote the first draft of the manuscript with support from DN, JA, PR, YG, SH, ID. All authors read and approved the final manuscript.
Funding
The authors did not receive any funding for the work in this manuscript.
Competing Interests
The authors have declared that no competing interests exists.
References
- World Health Organization. Depression. The World Health Organization Website; 2017. Available from: http://www.who.int/mediacentre/factsheets/fs369/en/.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006; 3: e442. [CrossRef]
- IsHak WW, Greenberg JM, Balayan K, Kapitanski N, Jeffrey J, Fathy H, et al. Quality of life: the ultimate outcome measure of interventions in major depressive disorder. Harv Rev Psychiatry. 2011; 19: 229-239. [CrossRef]
- IsHak WW, Mirocha J, James D, Tobia G, Vilhauer J, Fakhry H, et al. Quality of life in major depressive disorder before/after multiple steps of treatment and one-year follow-up. Acta Psychiatr Scand. 2015; 131: 51-60. [CrossRef]
- Group, T. W. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998; 46: 1569-1585. [CrossRef]
- Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006; 163: 28-40. [CrossRef]
- Parker G, Graham R, Sheppard E. The treatment of nonmelancholic depression: when antidepressants fail, does psychotherapy work? Can J Psychiatry. 2014; 59: 358-365. [CrossRef]
- Pigott HE, Leventhal AM, Alter GS, Boren JJ. Efficacy and effectiveness of antidepressants: current status of research. Psychother Psychosom. 2010; 79: 267-279. [CrossRef]
- Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol. 2012; 80: 547-559. [CrossRef]
- van Leeuwen RW, Swart EL, Boom FA, Schuitenmaker MS, Hugtenburg JG. Potential drug interactions and duplicate prescriptions among ambulatory cancer patients: a prevalence study using an advanced screening method. BMC Cancer. 2010; 10: 679. [CrossRef]
- Kessler RC, Soukup J, Davis RB, Foster DF, Wilkey SA, van Rompay MI, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001; 158: 289-294. [CrossRef]
- Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998; 280: 1569-1575. [CrossRef]
- Norcross JC, Pfund RA, Prochaska JO. Psychotherapy in 2022: A Delphi poll on its future. Prof Psychol-Res Pr. 2013; 44: 363-370. [CrossRef]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008; 12: 163-169. [CrossRef]
- Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, et al. Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep). 2007; 155: 1-263.
- Nauriyal DK, Drummond MS, Lal YB. Buddhist thought and applied psychological research: Transcending the boundaries. London: Routledge; 2006. (pp229-249).
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982; 4: 33-47. [CrossRef]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: A proposed operational definition. Clin Psychol Sci Pract. 2006; 11: 230-241. [CrossRef]
- Kabat-Zinn, J. Wherever you go there you are: Mindfulness meditation in everyday life. New York: Hyperion; 1994.
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol Sci Pract. 2003; 10: 125-143. [CrossRef]
- Tang YY, Posner MI. Theory and method in mindfulness neuroscience. Soc Cogn Affect Neurosci. 2012.
- Hart W. The art of living - Vipassana meditation as taught by S.N. Goenka. Pariyatti. 1987.
- Ivanovski B, Malhi GS. The psychological and neurophysiological concomitants of mindfulness forms of meditation. Acta Neuropsychiatr. 2007; 19: 76-91. [CrossRef]
- Grossman P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology's (re)invention of mindfulness: comment on Brown et al. Psychol Assessment. 2011; 23: 1034-1040. [CrossRef]
- Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002; 64: 71-83. [CrossRef]
- Coelho HF, Canter PH, Ernst E. Mindfulness-based cognitive therapy: evaluating current evidence and informing future research. J Consult Clin Psychol. 2007; 75: 1000-1005. [CrossRef]
- Kabat-Zinn J, Hanh, T. N. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta. 2009.
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, et al. Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clin Psychol Rev. 2018; 59: 52-60. [CrossRef]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014; 174: 357-368. [CrossRef]
- Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G, et al. Efficacy of Mindfulness-Based Cognitive Therapy in Prevention of Depressive Relapse: An Individual Patient Data Meta-analysis From Randomized Trials. JAMA Psychiatry. 2016; 73: 565-574. [CrossRef]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010; 78: 169-183. [CrossRef]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013; 33: 763-771. [CrossRef]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004; 57: 35-43. [CrossRef]
- Chiesa A, Malinowski P. Mindfulness-based approaches: are they all the same? J Clin Psychol. 2011; 67: 404-424. [CrossRef]
- Gunaratana BH. Mindfulness in plain English: 20th Anniv. Boston: Wisdom Publications; 2011.
- Kapleau P, Smith H. The Three pillars of Zen: teaching, practice, and enlightenment: Harper & Row; Boston: Bacon Press; 1966. (214 p).
- Kabatzinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness (15th anniversary ed.). New York: Dell Publishing; 2014.
- Segal ZJ, Williams MG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapses. New York: Guildford Press; 2002.
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999.
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. CurrPsychiat Rep. 1993; 6: 225-231.
- Surawy C, Roberts J, Silver A. The effect of mindfulnesstraining on mood and measures of fatigue, activity, and quality of life in patients with chronic fatigue syndrome on a hospital waiting list: A series of exploratory studies. Behav Cogn Psychoth. 2005; 33: 103-109. [CrossRef]
- Schutze R, Slater H, O'Sullivan P, Thornton J, Finlay-Jones A, Rees CS. Mindfulness-Based functional therapy: a preliminary open trial of an integrated model of care for people with persistent low back pain. Front Psychol. 2014; 5: 839.
- Maharishi Mahesh Yogi. Maharishi mahesh yogi on the bhagavad gita. New York: Penguin Books; 1969.
- Toneatto T, Nguyen L. Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research. Can J Psychiatry. 2007; 52: 260-266. [CrossRef]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6: e1000097. [CrossRef]
- Higgins J, Green SE. Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration (Eds). Naunyn-Schmiedeberg's Arch. Pharmacol. 2011; 5: S38.
- Pagnini F, Marconi A, Tagliaferri A, Manzoni GM, Gatto R, Fabiani V, et al. Meditation training for people with amyotrophic lateral sclerosis: a randomized clinical trial. Eur J Neurosci. 2017; 24: 578-586. [CrossRef]
- la Cour P, Petersen M. Effects of mindfulness meditation on chronic pain: a randomized controlled trial. Pain Med. 2015; 16: 641-652. [CrossRef]
- Chiesa A, Castagner V, Andrisano C, Serretti A, Mandelli L, Porcelli S, et al. Mindfulness-based cognitive therapy vs. psycho-education for patients with major depression who did not achieve remission following antidepressant treatment. Psychiatry Res. 2015; 226: 474-483. [CrossRef]
- Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, Hebert JR. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Res Treat. 2012; 131: 99-109. [CrossRef]
- Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. J Clin Psychol. 2012; 68: 715-731. [CrossRef]
- Chiesa A, Mandelli L, Serretti A. Mindfulness-based cognitive therapy versus psycho-education for patients with major depression who did not achieve remission following antidepressant treatment: a preliminary analysis. J Altern Complement Med. 2012; 18: 756-760. [CrossRef]
- Gaylord SA, Palsson OS, Garland EL, Faurot KR, Coble RS, Mann JD, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol. 2011; 106: 1678-1688. [CrossRef]
- Wong SY, Chan FW, Wong RL, Chu MC, Kitty Lam YY, Mercer SW, et al. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: a randomized comparative trial. Clin J Pain. 2011; 27: 724-734. [CrossRef]
- Gross CR, Kreitzer MJ, Reilly-Spong M, Wall M, Winbush NY, Patterson R, et al. Mindfulness-based stress reduction versus pharmacotherapy for chronic primary insomnia: a randomized controlled clinical trial. Explore. 2011; 7: 76-87. [CrossRef]
- Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain. 2011; 152: 361-369. [CrossRef]
- Godfrin KA, van Heeringen C. The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: A randomized controlled study. Behav Res Ther. 2010; 48: 738-746. [CrossRef]
- Grossman P, Kappos L, Gensicke H, D'Souza M, Mohr DC, Penner IK, et al. MS quality of life, depression, and fatigue improve after mindfulness training: a randomized trial. Neurology. 2010; 75: 1141-1149. [CrossRef]
- Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, et al. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Altern Ther Health Med. 2010; 16: 30-38
- Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JM. Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behav Res Ther. 2009; 47: 366-373. [CrossRef]
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol. 2008; 76: 966-978. [CrossRef]
- Moritz S, Quan H, Rickhi B, Liu M, Angen M, Vintila R, et al. A home study-based spirituality education program decreases emotional distress and increases quality of life--a randomized, controlled trial. Altern Ther Health Med. 2006; 12: 26-35.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017; 358: j4008. [CrossRef]
- Pies R. Are antidepressants effective in the acute and long-term treatment of depression? Sic et Non. Innov Clin Neurosci. 2012; 9: 31-40.
- Solati K, Mousavi M, Kheiri S, Hasanpour-Dehkordi A. The Effectiveness of Mindfulness-based Cognitive Therapy on Psychological Symptoms and Quality of Life in Systemic Lupus Erythematosus Patients: A Randomized Controlled Trial. Oman Med J. 2017; 32: 378-385. [CrossRef]
- Gallo R, Chiorri C, Gasparini G, Signori A, Burroni A, Parodi A. Can mindfulness-based interventions improve the quality of life of patients with moderate/severe alopecia areata? A prospective pilot study. J Am Acad Dermatol. 2017; 76: 757-759. [CrossRef]
- Lee CE, Kim S, Kim S, Joo HM, Lee S. Effects of a Mindfulness-Based Stress Reduction Program on the Physical and Psychological Status and Quality of Life in Patients With Metastatic Breast Cancer. Holist Nurs Pract. 2017; 31: 260-269. [CrossRef]
- Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psychiatry. 2001; 23: 183-192. [CrossRef]
- Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med. 2010; 40: 1239-1252. [CrossRef]
- Davis DM, Jeffrey AH. What are the benefits of mindfulness. APA Monitor on Psychology. 2012; 43: 64.
- Lamers SM, Bolier L, Westerhof GJ, Smit F, Bohlmeijer ET. The impact of emotional well-being on long-term recovery and survival in physical illness: a meta-analysis. J Behav Med. 2012; 35: 538-547. [CrossRef]
- Chambers SK, Occhipinti S, Foley E, Clutton S, Legg M, Berry M, et al. Mindfulness-Based cognitive therapy in advanced prostate cancer: A randomized controlled trial. J Clin Oncol. 2017; 35: 291-297. [CrossRef]
- Paller CJ, Campbell CM, Edwards RR, Dobs AS. Sex-based differences in pain perception and treatment. Pain Med. 2009; 10: 289-299. [CrossRef]


