Evaluating a 3-Week Model for Reducing Symptoms of Stress in Traumatised Youth Using the Trauma Tapping Technique (TTT) for Self-help: A Pilot Trial
Peta Stapleton 1, * ![]() , Ulf Sandstrom 2
, Ulf Sandstrom 2 ![]() , Gunilla Hamne 2
, Gunilla Hamne 2 ![]()
- School of Psychology, Bond University, Queensland, Australia
- Peaceful Heart Network, Upplandsgatan 6, 111 23 Stockholm, Sweden
* Correspondence: Peta Stapleton ![]()
Academic Editor: Gerhard Litscher
Received: September 12, 2018 | Accepted: December 17, 2018 | Published: December 24, 2018
OBM Integrative and Complementary Medicine 2018, Volume 3, Issue 4 doi: 10.21926/obm.icm.1804036
Recommended citation: Stapleton P, Sandstrom U, Hamne G. Evaluating a 3-Week Model for Reducing Symptoms of Stress in Traumatised Youth Using the Trauma Tapping Technique (TTT) for Self-help: A Pilot Trial. OBM Integrative and Complementary Medicine 2018; 3(4): 036; doi:10.21926/obm.icm.1804036.
© 2018 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Background: This pilot trial investigated whether a 3-week self-help model for stress reduction using the Trauma Tapping Technique (TTT) would impact traumatized youth in the Democratic Republic of the Congo on post-traumatic stress symptoms and general happiness. It also focussed on the acceptability of the program to recipients and implementation in a community with complex trauma and conflict.
Methods: The study involved 77 youth who received a TTT 3-week model of intervention (self-applied). Post traumatic stress symptoms and general happiness were assessed pre and post the intervention and at 6-month follow-up.
Results: TTT was associated with a significantly greater improvement in happiness (12.12% increase, p<0.05) and a significant reduction in trauma symptomology from pre- to immediately post-test (6% decrease, p<0.05). The 6-month results were nonsignificant (p=0.056) however from pre to follow-up, participants indicated an 11.4% reduction in their trauma symptoms. The qualitative investigation of staff and participants revealed the intervention had a positive effect on trauma stress symptoms and happiness outcomes findings.
Conclusions: The proposal that a 3-week model of teaching emotional literacy via a self help technique such as TTT is a potential solution for complex communities is discussed, and suggestions for future large scale trials are offered.
Keywords
Trauma; youth; tapping; stress; post traumatic stress; peer-to-peer; self-help; self-regulation; emotional literacy; psychosocial support
1. Introduction
One of the biggest challenges to individual mental health and wellbeing as well as conflict resolution and peace building processes in the footsteps of war and genocide is trauma, or specifically post traumatic stress reactions. The prevalence of Post Traumatic Stress Disorder (PTSD) and its common perception as a treatment resistant and refractory condition, has led to extensive investigation of treatments that might ameliorate PTSD symptoms. Most current treatments involve expert assisted sessions (recommendations range from eight to 16 sessions), or medication. The evidence based psychotherapies recommended by the American Department of Veteran Affairs include: 1. Prolonged Exposure (PE) which involves talking about the trauma and addressing avoidance behaviors; 2. Cognitive Processing Therapy (CPT) which teaches someone how to reframe negative thoughts about the trauma; 3. Eye-Movement Desensitization and Reprocessing (EMDR) which is a way to process and make sense of the trauma while paying visual attention to a back-and-forth movement or sound; and Medications typically prescribed for depression and anxiety (e.g. Sertraline, Paroxetine, Fluoxetine, Venlafaxine).
All of these psychotherapeutic or medical interventions require expert training, and administration. They are not usually viable options in areas of post-conflict where large populations are living with trauma and often in traumatizing conditions. The lack of infrastructure and organized health care as well as insecurity, language barriers, living conditions and cultural differences contribute to make these interventions unworkable and often impracticable. To pay for medication is a challenge but also financing transportation to a treatment. There is a need for an intervention that can be taught peer-to-peer on a community level, to reach as many as possible from a village health and First Aid perspective.
Thus a goal of the current study was to investigate a 3-week model based on emotional literacy about symptoms of stress and trauma, and a self-applied stress reduction intervention that has previously proven effective in reducing symptoms of PTSD, to youth in a traumatised conflict area. The overarching goal was to ascertain the ability of the technique as a community-led approach.
1.1 Thought Field Therapy
Thought Field Therapy (TFT) originally emerged in the 1980s [1] and is considered a precursor to Emotional Freedom Techniques (EFT) [2] and the Trauma Tapping Technique (TTT) used in this 3-week model.
TFT involves tapping on acupoints on the body and is focused on specific sequences of acupoints for different emotional problems, rather than the one model fits all approach of EFT. The effectiveness of TFT with a range of civilian and war survivors has been explored [3,4]. TFT has also been added to the Substance Abuse and Mental Health Services Administration’s National Registry of Evidence-based Programs and Practices, as effective for trauma and stressor-related disorders and symptoms, self-regulation and personal resilience/self-concept.
A single session of TFT was offered to 50 orphaned adolescents and genocide survivors, who had been suffering with symptoms of PTSD since the Rwandan genocide 12 years earlier [5]. Their symptoms significantly decreased (p < .0001), and informal interview with the adolescents and the caregivers, indicated dramatic reductions of PTSD symptoms such as flashbacks, nightmares, bedwetting, depression, isolation, difficulty concentrating, jumpiness, and aggression. Following the study, self and peer use of TFT became part of the culture at the orphanage, and at one-year follow-up the initial improvements had been maintained.
An investigation of 145 adult survivors from the 1994 genocide in Rwanda, randomly assigned participants to a TFT treatment or a waitlist control group [6]. The group who received TFT experienced reduced trauma symptoms on all measures, and this was sustained at two-year follow-up. Community-based partnerships of trained TFT mental health practitioners and community leaders have also been successful. Rwandan community leaders, who provided one-time individual trauma-focused TFT interventions to 164 adult survivors of the 1994 Rwandan genocide in their native language (Kinyarwanda) randomly allocated participants to an active TFT group or a waitlist control group. The waitlist did receive the TFT treatment as well, but not until after the active treatment was complete. Each participants was treated an average of 3.19 times and significant differences were found for trauma symptoms and level of PTSD symptom severity and frequency between the treatment and the waitlist control groups. Large effect sizes (from .8 to 1.33) were found between the treatment and no treatment control conditions on the subscales of Anxious Arousal, Depression, Anger/Irritability, Intrusive Experiences, Defensive Avoidance, Impaired Self-Reference, and Dissociation (Trauma Symptom Inventory) and the Modified Posttraumatic Stress Disorder Symptom Scale frequency and severity scales. Outcomes suggested that a one-time, community leader facilitated trauma-focused TFT intervention may be beneficial with protracted PTSD in genocide survivors.
Finally, a meta analysis of five TFT studies found the overall effect size for the pre- to post-TFT treatment conditions was extremely large and statistically significant (-2.27) [7]. While the authors concluded TFT was highly effective in reducing trauma symptoms in a variety of populations and settings, they did acknowledge limitations of the review. The methodology of the studies included were different to each other, and not every study was included. Because of the small number of experienced and approved TFT trainers, and limited funding available for large-scale randomized controlled studies, the quality of studies published may be compromised.
1.2 Emotional Freedom Techniques
Emotional Freedom Techniques (EFT) emerged from TFT. EFT combines elements of established methods such as exposure and cognitive therapies with somatic stimulation in the form of acupressure. A meta-analysis of seven studies investigating EFT in the treatment of PTSD found a very large treatment effect (weighted Cohen’s d = 2.96, 95% CI 1.96-3.97; p < 0.001) for the studies that compared EFT to usual care or a wait list [8]. In addition, a systematic review assessing the evidence for 15 new or novel interventions for the treatment of PTSD found there were four interventions that had moderate quality evidence from randomized controlled trials, and one of these was EFT [9].
EFT is often referred to as ‘tapping’ as it uses a two-finger tapping process on acupoints on the body, in conjunction with a cognitive acceptance statement. Subjects typically rate their level of distress on a scale of 0 to 10 (Subjective Units of Distress) [10], and then state their issue in a setup statement with an acceptance element. An example would be “Even though I feel angry right now (or another issue), I deeply accept myself anyway”. There are eight acupoints on the face and upper body used in the tapping process that follows, and a shorter reminder phrase is repeated for engagement as the person taps (e.g. feel angry). With roots in Eastern philosophies, particularly acupuncture, we now understand that EFT has profound effects on the nervous system, the production of stress hormones (particularly cortisol), DNA regulation, and brain activation.
1.3 EFT for Trauma Conditions
An initial study of veterans meeting the clinical criteria for PTSD, were randomly assigned to either a six-hour EFT treatment (n=30) or standard care (n=29). Those who met the clinical criteria for PTSD and received the EFT intervention had significant reductions in psychological distress and PTSD symptoms. Following both treatments, 90 percent of those who received EFT no longer met criteria for PTSD, compared to only four percent in wait-list standard care group. Three months later, 86 percent of those who received the EFT intervention remained in remission, whilst 80 percent remained in remission at six-months [11].
Another examination of 16 returned war veterans with PTSD who received 10 hour-long EFT sessions, found a significant reduction in interleukin expression (responsible for the regulating the body’s inflammation response). Genes associated with improved functioning of the immune system were up regulated and there was a significant association between improvement in the veterans’ mental health symptoms and positive changes in the expression of their genes related to stress hormones [12].
An investigation of EFT for subclinical PTSD symptoms to reduce risk of a later diagnosis, tracked 21 veterans [13] who were randomized into a treatment as usual (TAU) wait-list group and an experimental group, who received TAU plus six sessions of EFT. The TAU group had no changes during the waiting period, and then they received the EFT treatment at the end of this period. For the collapsed groups after treatment, the mean score of 25 indicated a 64 percent reduction in symptoms. The veterans maintained their gains at three- and six-month follow-up, with a large treatment effect (d = 1.99). The study also showed reductions in traumatic brain injury symptoms and insomnia.
Finally, a comparison of Cognitive Behavioural Therapy (CBT) and EFT for 50 internally displaced female refugees who had been victims of sexual gender-based violence (SGBV) in the Democratic Republic of Congo found after two 2.5-hour treatment sessions per week for four consecutive weeks (eight sessions in total), all women indicated significant post-test improvement in both groups on measures of trauma, PTSD symptoms and general mental health [14]. The women also maintained their gains whether treated with EFT or CBT, and overall demonstrated the effectiveness and non-inferiority of EFT to a gold standard intervention.
1.4 The Current Study
Researchers [15] have pointed out the incongruity between the demands for evidence-based practice and the fact that most evidence-based recommendations for behavioural interventions are derived from highly controlled efficacy trials. When there are few published studies or existing data on an existing intervention, and when practitioners call for more studies in real-world settings, then pilot studies are useful. This study particularly addressed the areas of acceptability to the participants, the implementation of the program in a conflict zone, the adaptation of the technique with different populations to those already examined.
Trauma Tapping Technique (TTT) used in the current study was developed in collaboration with Dr Carl Johnson in Rwanda specifically for traumatized populations. It was inspired by his experiences of using TFT with survivors of the war in Kosovo and simplified to work with a low level of expertise. TTT is a combination of TFT and EFT in combination with a breathing exercise that is derived from the tactical breathing or box breathing used in American military and police trainings and breathing techniques from mindfulness and yoga. TTT has been designed specifically to keep spoken interventions at a minimum which makes it different from EFT and simple to remember. This facilitates lay learning and maintains the integrity of individual experiences which makes it possible to spread peer-to-peer in communities in challenged areas, in this study specifically the Eastern Democratic Republic of Congo.
The minimum requirement of spoken interventions makes it possible to deliver TTT in groups and to avoid re-traumatization by verbally revisiting traumatizing memories (which occurs in many traditional exposure approaches). TTT has been taught in a TTT 3-week model to groups of adolescent survivors of the genocide in Rwanda and acts of war and gender based violence in Democratic Republic of the Congo, Sierra Leone, Chad and more than ten other countries since 2007.
The complete instruction for applying TTT is: “Connect ever so lightly to what bothers you and tap 10-15 times on the points 1-14 (see Figure 1) with two fingers, firmly and precisely. Take a deep breath, hold it, breathe out and relax. Repeat the breath. Then repeat the full procedure once again.” The tapping can be self-applied or administered by another person.
This is the first study to preliminarily evaluate the results of the TTT 3-week model for traumatized youth. This study aimed therefore, to investigate the effect of group trainings of TTT in this model, for traumatized youth in the DR Congo, on post-traumatic stress symptoms and general happiness.
2. Materials and Methods
Ethical approval was obtained for the current study from the lead author’s affiliated university at the time. The school principal, parents and guardians also gave consent and approval for all youth involved.
2.1 Recruitment and Participants
There were two groups included in the current study. One group included 24 male and 24 female youth, aged 10 to 30 years who self-selected to the intervention program from a rehabilitation centre where they attended school (n= 48; 68.8%). The Transit and Orientation Center (Centre de Transit et d’Orientation) of the organization BVES is designed for children demobilised from armed forces and groups in the area Eastern Congo. Typically, these youth have no parents due to war conditions, therefore the Director of the Centre provided all consent for their participation.
The BVES (Bureau pour le Volontariat au service de l’Efance et de la Santé) is a Congolese national non-profit organization with its headquarters in Bukavu, South Kivu province in the east of the country. It was created by a group of multidisciplinary volunteers in the 1990s to counter the deterioration of the situation for children in the Congo with the birth of armed conflicts in the eastern part of the country. Since then, the BVES has been involved in the defence, promotion and protection of the rights of children, focusing on all vulnerable children: street children, refugee children, unaccompanied children, children in conflict with the law, children working in the mines, children associated with the armed forces and armed groups as well as sex slaves and girls and boys subjected to sexual violence.
The second group included 19 male and 10 female young people in the same area of conflict and stressful daily life at the Karhana High School (n=29; 37.7%). Youth took part with the support and authorization of school officials and with parental consent.
In total 77 youth were recruited through self-selection and completed the three-week TTT model. The age range was 10 to 30 years (M=15.98 years, SD = 2.56). There were 45 males (58.5%) and 32 females (41.5%) in total across the two sites. A power analysis using G*Power [12] indicated that, with a two-sided significance of 0.05 and a power of 0.8, a total of 51 participants would be required. The sample size in the current study was adequate to achieve this.
2.2 Procedure
Ethical approval for the study was granted by the Bond University Human Research Ethics Committee, and all involvement in the study was voluntary. The Director of the BVES Centre provided consent for youth who participated and, in the school group both parents and the school principal provided consent. All youth understood they could withdraw at any time and had access to usual counselling services by psychosocial staff and medical doctors in if they needed further support. There were no reported cases of anyone needing this.
All measures were converted into French or Swahili as per the local languages, and checked again for interpretation, by an expert translator. The youth completed the measures in paper form at the start of the first session, at the end of the three-week program, and after a 6-month follow-up.
Trauma experts and the founders of the Peaceful Heart Network (second and third authors) delivered the trauma tapping technique together with the local psychologists and social workers at the rehabilitation centre and another trauma expert and local social worker at the schools during the initial training day. After this the children would perform a daily tapping session of 10-20 minutes together led by a staff or one of themselves during the next 3-weeks.
2.3 Measures
The PTSD Checklist (PCL-5) [13] was used to assess symptoms in relation to generic “stressful experiences”. It is suitable for any population, and simplifies assessment based on multiple traumas because symptom endorsements are not attributed to a specific event [14]. It is a 17-item self-report measure that assesses the 17 diagnostic symptoms of PTSD (Diagnostic and Statistical Manual of Mental Disorder) and uses a 0-4 rating scale for each symptom. Rating scale descriptors are: "Not at all," "A little bit," Moderately," "Quite a bit," and "Extremely." The total symptom severity score range is 17 to 80.
The PCL-5 asks how much someone has been bothered by a certain problem in the last month, for example: “Having physical reactions (e.g., heart pounding, trouble breathing, or sweating) when something reminded you of a stressful experience from the past?”, and “Avoid thinking about or talking about a stressful experience from the past or avoid having feelings related to it?” The PCL-5 has demonstrated good retest reliability [15] and internal consistency (all over .75) has been found in 14 studies examining psychometrics in military samples, adults with severe mental illness, dually diagnosed patients with HIV, women with substance use disorders, women treated for breast cancer, adults with recent limb loss, female undergraduates, and community adults [16].
A 10 –item happiness scale was also used to measure participants’ general life satisfaction and was scored one to five (one being the lowest and five being the highest). Questions included: “How often do you laugh?”, “How often does somebody help you?”, and “How easily do you recover from failures or criticism?” The happiness scale was developed for the local culture as there was not an existing measure that could be used, nor one that made sense in this cultural context.
Finally, a qualitative questionnaire was used to elicit participant reflections of the impact of the TTT program, and observations of the teachers and carers attached to them in the school group. The school only participated in this aspect as the BVES Centre was for children demobilised from armed forces and groups and typically these youth have no parents due to war conditions, only a Director of the Centre.
2.4 Trauma Tapping Technique Three-Week Model
Youth engaged in an initial two-hour treatment group session. The treatment session covered the theory and symptoms relating to trauma, self-application of the tapping technique, the breathing instruction, and the use of song for easy memory recall of the technique. It was demonstrated by the therapists and self-applied by the youth attending. After this the participants practised the self-application of tapping under supervision as a daily routine during the ensuing three weeks. They were encouraged to continue using the technique after the intervention period ended.
The tapping technique included applying pressure with a tapping process (using two fingers) on acupoints on the upper body, hands and face, after focusing on a distressing feeling or memory (see Figure 1). A “subjective units of distress” (SUD) [6] rating was used at the start of the process (10=extreme distress; 0=no distress), and at the end of two rounds of tapping.
The actual sessions proceeded as such: an initial explanation of the origin of the TTT was given by the TTT facilitators, its history and its advantages as well as its therapeutic indication were then covered. They provided a brief overview on trauma and psychological stress. They discussed the TTT technique used a "learning by doing" methodology and offered a demonstration of the technique, which then led to practice by the participants. Students worked in pairs using the technique and the facilitators offered any corrections as needed.
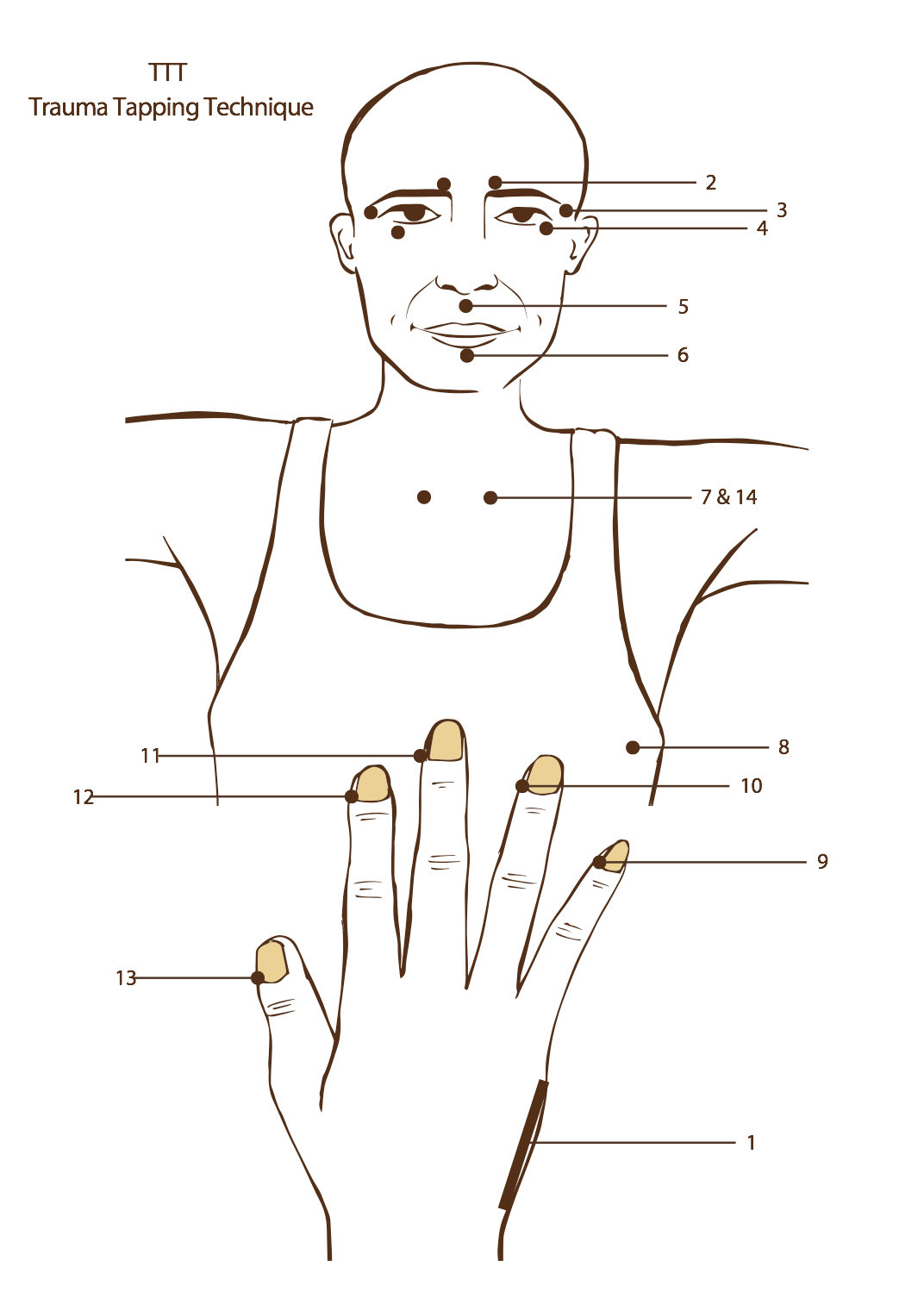
Figure 1 Tapping points.
3. Results
3.1 Quantitative Analyses
The IBM Statistical Package for Social Sciences (SPSS) Version 26 was used for analyses. Chi-square analyses were used to determine if the demographic characteristics of age and gender differed between the two groups prior to the intervention. Results revealed that there were between groups difference for age χ2 (22) = 31.77, p = .08 and gender χ2 (2) = 42.47, p = .00. There were more participants between the ages of 15 and 17 years in the Centre group, and more males in the school group. These were not considered to be problematic as all groups were collapsed for the final analyses.
To test whether TTT had an immediate effect on the outcomes of interest, two separate repeated ANOVAs were conducted to measure the effect of two levels of the repeated measure variable of time (pre-test versus post-test) and comparison at 6-months for the PCL. The 77 participants were analysed as a single group. Associated means at each of the time points are presented in Table 1.
Table 1 Collapsed group mean scores and standard deviations for the dependent variables across time, including 95% confidence.
|
Variable |
Group Means |
95% CI |
||
|
M |
SD |
Lower |
Upper |
|
|
PCL (Baseline) |
37.70 |
15.46 |
32.45 |
43.12 |
|
PCL (Post) |
33.29 |
14.65 |
21.64 |
26.41 |
|
PCL (6month) |
29.96 |
11.68 |
25.84 |
34.15 |
|
Hap (Baseline) |
18.77 |
10.15 |
15.25 |
22.22 |
|
Hap (Post) |
24.00 |
7.11 |
21.64 |
26.41 |
Note. PCL = PTSD Checklist. Hap= Happiness measure. 95% CI = 95% confidence intervals for the total mean scores.
It should be noted that that pre-treatment mean (33.37) of the PCL-5 indicated provisional diagnoses of PTSD was likely [13], and thus this sample was indeed experiencing a high level of trauma symptoms.
Assumptions of normality were met for the PCL. There was a significant reduction from pre- to post-test in PCL symptomology (p=0.02; 6% decrease, see Table 2). At pre, the PCL-C score average was 37.70 (and suggested cutoffs indicated they were experiencing PTSD). Research also suggests that a five to 10 point change is reliable and a 10-20 point change is clinically meaningful [17]. It is recommended to use five points as a minimum threshold for determining whether an individual has responded to treatment and 10 points as a minimum threshold for determining whether the improvement is clinically meaningful. There was a decrease of 7.74 points in this study over 6-months, indicating participants were responding to the treatment.
Assumptions of normality were met for the Happiness measure. There was a significant change from pre- to post-test in happiness symptoms, indicating it increased by 12.12% (p=0.00; see Table 2).
Table 2 Means, standard deviations and repeated measure ANOVAs for treatment group at pre-, post-treatment and 6-month follow-up.
|
|
|
Pre-treatment |
Post-treatment |
6-month |
df |
F |
p |
|||
|
|
N |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
|
|
PCL |
77 |
33.37 |
16.06 |
28.51 |
16.33 |
29.96 |
11.68 |
(1, 63) |
10.77 |
0.002 |
|
Happ |
77 |
17.15 |
13.07 |
22.00 |
12.58 |
- |
- |
(1, 63) |
179.02 |
0.00 |
Note. PCL = PTSD Checklist. Hap= Happiness measure.
3.2 Follow-up Analyses
For the collapsed group, 31 participants completed the 6-month follow-up for the PCL-C only and this was due to the transient nature of the communities and youth no longer being available to be contacted. This movement is not unusual in these populations.
The significant reduction from pre-treatment to post-treatment for PCL scores approached significance at the 6-month follow up (M=29.96, SD=, p=.056), and from pre to 6-months participants still reported a decrease of trauma symptoms by 11.4%. Research suggests that a 5-10 point change represents reliable change, and recommends to use 5 points as a minimum threshold for determining whether an individual has responded to treatment. This sample approached that difference from pre to post treatment (-4.86).
3.3 Qualitative Data
For monitoring and qualitative evaluation, the TTT facilitators interviewed the Karhana High School prefect of studies (HeadMaster), parents' representatives, teachers and students themselves on the level of satisfaction with the positive effects or impacts of TTT.
All indicated a significant change occurred in the children after the TTT intervention.
"We struggled to control and contain children in class; each time there was violence, brawl, intolerance, mistrust between students themselves and against us teachers, several cases of irregularities and absences due to the symptoms of pathologies that often people did not know the diagnosis and even less the etiology or causes. A drop in school performance, which resulted in poor classroom results, less concentration in class and many other difficulties that arose in the classroom, at school or in family / community. Today we can breathe, we now constitute "a school friend of children and young people" because a kind of atmosphere has already existed since this half of the year, I am sure and it is thanks to TTT that it happens. Otherwise, no school in our community has ever defeated a period and such a generation for nearly two decades.” (HeadMaster).
The school indicated an openness to continuing to use TTT as part of the ongoing program, and also noted a decrease in school refusal and failure. “We have gradually observed an incredible decrease in violence and aggression at school whether it be on the part of pupils or teachers. TTT has made many applications for registration to our school thanks to this improved relationship and the results obtained by the students since last year when TTT was introduced in our school. There has been a noticeable decrease in cases of failure and school dropout that we evaluated at more than 63.4%, record that no school in the area has ever reached. We will make TTT an essential and educational activity that sanitary in our school and for our children from next year, we will integrate it into the local curriculum as a course of education for life and health in all grades and classes and we had already decided in the school management and technical committee meeting after the significant results obtained during the evaluation of the impact” (Prefect school representative).
A parent representative also indicated the same: "Whether at school or with the family, the children have significantly changed their behavior and are no longer those little devils we knew about 6 months ago but rather little angels that we like to see and live with. This curse that we thought, these demons to which we linked the behavior of our students disappeared from a simple joke acquired for free because we have not paid anything or sacrificed, only happy to see our children become these children where we wanted.” (Parent representative).
The students themselves confirmed this: “I could not be able to sleep or enter a house alone, I feared day and night. I felt as if something bad had happened to me, sometimes I screamed because I saw things, extra-terrestrial that others around me did not see. I had difficulty reading my classes because I could start a page and I would even do more than two hours without finishing it or understand what I read because my ideas were still elsewhere, carried away by I do not know. Not what. Now, this is not the case anymore. No! This has completely ended, I am free and updated. I went to see the marabouts and went to the prayer rooms several times but in vain until I did TTT. For me, TTT is a meal I take every day.” (student, aged 15).
“I was in prison 10 months with hard labor and no food for weeks. I was there for having been in an armed group. As punishment they would put us to clean latrines. I would not sleep since I left the prison after 10 months. First I took TTT like a joke and I made it like a joke but then the trainer was explaining to me that it is a useful treatment that has helped a lot of people. I tried it to find out. TTT changed me because I could sleep. Also when I had a lot of thoughts in my mind I could do TTT to resolve them. I could not talk after prison, I was in a prison of my head, but with TTT I started talking. Now I also eat a lot more and have grown in a healthy way.” (Olivier Igiraneza 16 yrs ).
Similar comments from others included:
“When I did TTT since June I started to feel the joy of living and to design ideas and plan B of life, the need to live close to others, love to others. TTT has made people get closer to me and some people tell me that I have completely changed, that I have become a good person and I am proud of it.” (student, aged 16).
“On this day it is as if I was reborn, I went through a period when my head hurt so much that all the medicines prescribed to me were unsuccessful. I went to bed without sleeping because of intrusive dreams that disturbed my night and made me spend my nights under the stars. Currently these problems are gone and I feel in my best life.” (student, aged 15).
“I no longer lived at home, my parents had driven me away because I already lived like a wild beast, my reactions to my brothers, sisters and comrades were violent and stupid, my thoughts and words were unbearable and my behavior in general was crazy. But a little while after I participated in TTT exercises my life gradually changed and at school I start making new friends, teachers call me a student now and my parents have told me that they can take me home again if I stay as I am.” (student, aged 16).
Comments from the BVES rehabilitation Center:
“I have been here 3 months and at Uvira as medical doctor and health responsible. I've seen the traumas here and very positive results from the Trauma Tapping Technique. They do it 2 times a week and when they come from army or street they are physically closed and cannot talk, they are stressed and don't want to integrate. With these sessions of TTT they become happy and playful with the music and the exercise - it is not so serious to participate. From the point of view of psychosocial help and medical point of view there is great and beneficial results in how they behave. Specially those who have insomnia come and say they are sleeping. He also learned it here from Placide and it has a place not only here but also in society and the normal educational system.
We are victims of conflict in this country as a whole, there is need for sensibilisation by doing seminars and inviting people from different parts of the society and to visit the hospitals. Though television of course. In education to give it to the teachers and the pupils. There are many things you can do like sports and music but at the end of the day the kids have not changed, with this (TTT) they have. It is a key for opening up.” (Dr Olivier Bonane Murhabazi, MD, health responsible at BVES).
The facilitators themselves offered these observations:
Challenges:
“We have taught stress regulation for self help and others to children liberated from the armed forces and school children of the same age living in the same violent and challenged society. During 10 years we have qualitative testimonials that show that those who have learned the techniques find them very helpful, life changing sometimes. The psychosocial staff, teachers and doctors involved with these children testify to the value and impact of the method. This study is an attempt to find out what the impact is on symptoms of trauma. The challenges involved are the lack of communication infrastructure (no internet, mail, phone), many language barriers, strange abstraction levels of questions in the PCL5 and the fact that many of the children sometimes simple disappear of the radar back into far away villages and sometimes into neighbouring countries in search of lost family or a job/school/better life. Regardless the fact that the study has a relatively small number of participants and the in exactitude of translating difficult questions over language, culture and abstraction levels, we find the results significant enough to recommend the model which has no costs and is spread peer to peer - and make more research.
Many of the participants were not skilled in reading and writing and not used to fill in forms. Since they have been forced in to the armed groups while very young they have missed school sometimes for several years. The questions were translated to Swahili which is one of the main languages in the area and the meaning of the questions had to be explained extensively.
One of the trainers of BVES read all the questions first in French and then in Swahili. Then another trainer explained in a more simple Swahili what the questions meant. It took somewhat more than an hour to fill in the form.
From this experience we also raise the question if these forms are the best way of measuring the level of PTS. As the qualitative interviews show the impact seems to exceed the quantitative measure.”
And finally, as the students and teachers all attested: “We ended up with a way of life positively appreciated by our entourage and envied by peers which attracts even several parents to want to enrol their children in this school …[TTT] has the ability to heal all members of our communities seriously affected by post-conflict trauma and end [it]. [We should] make TTT a common exercise that everyone can adopt and use”.
4. Discussion
In this geographical area of conflict, stress and post traumatic stress symptoms are real threat to public mental health and public security. Medication is available to very few because of cost and limited health care institutions. Access to counselors, therapists, psychologists and other mental health professionals is also extremely limited and there is an urge among global health visionaries to make simple tools of intervention accessible through the people already present (teachers, community leaders and health counsellors) according to the SUNDAR vision of Psychiatrist and global mental health expert Vikram Patel [18].
The TTT 3-week model may offer some solution to this problem. Administered with very little training and self-applied, TTT is to be considered as a psychological first aid technique. Findings of this pilot study indicate that the 3-week model resulted in a significant reduction of trauma symptoms and is clinically meaningful to the participants. The resulting increase in happiness symptoms was also significant. While the 6-month follow-up data was non-significant, the small sample size may account for that outcome. The lack of further outcome in the happiness scores may be to be expected due to ongoing traumatic living conditions, however the fact that the trauma symptoms approached significance at 6-months clearly indicated that symptomology was being affected. The staff, parents and the youth conferred by indicating the TTT 3-week model affected their physical and mental health and may have contributed to greater emotional stability.
The aims were met for this study. Certainly the acceptability of the intervention (how the intended individual recipients react to the intervention) was positive from all stakeholders. The implementation of the program was seamless and feedback encouraging, and given the existing research supporting community-led TFT trials in similar areas [2], the likelihood of TTT being disseminated amongst these neighbourhoods is high. The practicality of TTT being delivered when resources, time, commitment, or some combination thereof are constrained in some way, was also high. Finally, the adaptation of EFT and TFT for the targeted community highlights the potential success of already successful interventions with different populations.
4.1 Limitations
There are known challenges in conducting any study of interventions for mental health since there is little control over what happens in the lives of the participants outside the study, and in the current study of an unstable context it was even more so. Limitations of this study that may also decrease the generalizability of the findings include a small sample size, no random allocation of participants to conditions, and an absence of a comparison treatment. However, including both genders, consistent clinician delivery of the program, and the use of reliable and valid measures of trauma symptomology were strengths.
5. Conclusions
The results from this pilot study are important for widening the possibilities of empowering the patients and their families in an area of post-conflict with a simple model to decrease acute symptoms of PTSD. The results and feedback indicate at a preliminary level that the TTT 3-week-model can be a valid approach. Further studies are recommended with the above limitations addressed, including large scale randomised clinical trials.
Author Contributions
Dr Stapleton designed the trial and oversaw the delivery and analyses of data and writeup of publication. Mr Sandstrom and Ms Hamne delivered the intervention, arranged all consent and assisted with the writeup of the publication.
Funding
Association of Comprehensive Energy Psychology, USA.
Competing Interests
The authors have declared that no competing interests exist.
References
- Callahan RJ, Trubo R. Tapping the healer within: Using thought field therapy to instantly conquer your fears, anxieties, and emotional distress. Chicago, IL: Contemporary Books; 2011.
- Craig G. The EFT Manual (Emotional Freedom Techniques); 2007. Available at: http://www.emofree.com/
- Boath E, Rolling C. Echoes in bosnia and beyond. Somatic Psychother Today. 2015; 5: 38-41.
- Boath E, Stewart T, Rolling C. The impact of EFT and Matrix Reimprinting on the civilian survivors of war in Bosnia: A pilot study. Curr Res Psychol. 2014; 5: 64-72. [CrossRef]
- Sakai C, Connolly S, Oas P. Treatment of PTSD in Rwanda genocide survivors using Thought Field Therapy. Int J Emerg Ment Health. 2011; 12: 41-49.
- Connolly S, Sakai C. Brief trauma symptom intervention with Rwandan genocide survivors using Thought Field Therapy. International Int J Emerg Ment Health. 2011; 13: 161-172.
- Edwards J, Vanchu-Orosco M. A meta-analysis of randomized and nonrandomized trials of Thought Field Therapy (TFT) for the treatment of posttraumatic stress disorder (PTSD). Paper accepted at the Annual Meeting of the Association for Comprehensive Energy Psychology, San Antonio, Texas; 2017.
- Sebastian B, Nelms J. The effectiveness of Emotional Freedom Techniques in the treatment of posttraumatic stress disorder: A meta-analysis. Explore-J Sci Heal. 2016; 13: 16-25.
- Metcalf O, Varker T, Forbes D, Phelps A, Dell L, DiBattista A, Ralph N, O'Donnell M. Efficacy of fifteen emerging interventions for the treatment of Posttraumatic Stress Disorder: A systematic review. J Trauma Stress. 2016; 29: 88–92. [CrossRef]
- Wolpe J. The practice of behavior therapy. 2nd ed. New York, NY: Pergamon Press; 1973.
- Church D, Hawk C, Brooks AJ, Toukolehto O, Wren M, Dinter I, Stein P. Psychological trauma symptom improvement in veterans using EFT (Emotional Freedom Techniques): A randomized controlled trial. J Nerv Ment Dis. 2013; 201: 153-160. [CrossRef]
- Church D, Yount G, Rachlin K, Fox L, Nelms J. Epigenetic effects of PTSD remediation in veterans using Clinical EFT (Emotional Freedom Techniques): A randomized controlled pilot study. Am J Health Promot. 2018; 32: 112-122. [CrossRef]
- Church D, Sparks T, Clond M. EFT (emotional freedom techniques) and resiliency in veterans at risk for PTSD: A randomized controlled trial. Explore-J Sci Heal. 2016; 12: 355-365. [CrossRef]
- Nemiro A, Papworth S. Efficacy of two evidence-based therapies, Emotional Freedom Techniques (EFT) and Cognitive Behavioral Therapy (CBT) for the treatment of gender violence in the Congo: A randomized controlled trial. Energy Psychol Theory Res Treat. 2015; 7: 13-25. [CrossRef]
- Green L, Glasgow RE. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice based evidence? Am J Public Health. 2006; 96: 406–409. [CrossRef]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39, 175–191. [CrossRef]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. 2013; Available from: http://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress. 2015; 28: 489-498. [CrossRef]
- Conybeare D, Behar E, Solomon A, Newman M, Borkovec T. The PTSD checklist-civilian version: Reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol. 2012; 68: 699-713. [CrossRef]
- Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. 2011; 28: 596–606. [CrossRef]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: do clinicians and patients agree? Psychol Assess. 2008; 20: 131-138 [CrossRef]
- Patel V. SUNDAR: Mental health for all by all. BJPsych International. 2015; 12: 21–23. [CrossRef]


