Targeting Acute Islet Inflammation to Preserve Graft Mass and Long-Term Function
Carly M. Darden 1 ![]() , Srividya Vasu 2
, Srividya Vasu 2 ![]() , Kenjiro Kumano 2
, Kenjiro Kumano 2 ![]() , Bashoo Naziruddin 3
, Bashoo Naziruddin 3 ![]() , Michael C. Lawrence 2, *
, Michael C. Lawrence 2, * ![]()
- Institute of Biomedical Studies, Baylor University, Waco, TX, United States
- Islet Cell Laboratory, Baylor Scott and White Research Institute, Dallas, TX, United States
- Annette C. and Harold C. Simmons Transplant Institute, Baylor University Medical Center, Dallas, TX, United States
* Correspondence: Michael C. Lawrence ![]()
Academic Editor: Kåre I. Birkeland
Special Issue: Current Advancement of Islet Cell Transplantation in the Treatment of Diabetes Mellitus
Received: November 21, 2018 | Accepted: January 24, 2019 | Published: January 29, 2019
OBM Transplantation 2019, Volume 3, Issue 1 doi: 10.21926/obm.transplant.1901043
Recommended citation: Darden CM, Vasu S, Kumano K, Naziruddin B, Lawrence MC. Targeting Acute Islet Inflammation to Preserve Graft Mass and Long-Term Function. OBM Transplantation 2019; 3(1): 043; doi:10.21926/obm.transplant.1901043.
© 2019 by the authors. This is an open access article distributed under the conditions of the Creative Commons by Attribution License, which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is correctly cited.
Abstract
Islet transplantation is a minimally invasive cell based replacement therapy to prevent or reverse diabetes or hypoglycemia through natural hormonal responses to regulate blood glucose. However, extending the islet graft functional lifespan remains a challenge that prevents long-term success and widespread use of the procedure. Islets are subject to stress and damage and undergo immunological assault during transplantation procedures. Current treatments to prevent immune reactivity toward the graft come with toxic side effects, and damage to islets and loss of graft function still occurs. Accumulating evidence suggests that acute inflammatory reactions contribute to a significant loss of islet cell mass early in the transplant process. Inflammatory reactions involving a blood coagulation cascade and communication between islet cells and immune cells can destroy more than half the islet mass. These cyclic events link innate and adaptive immune responses that lead to graft failure. In this review, we discuss key components and strategies to target islet cell inflammation and delink the progression of inflammatory islet-immune cell responses that contribute to islet graft destruction.
Keywords
Islet cell transplantation; innate immune response; adaptive immune response; acute inflammation; IBMIR
1. Introduction
Islet transplantation represents a promising cell replacement therapy to prevent or reverse diabetes mellitus and is currently performed in select patients with uncontrollable type 1 diabetes or chronic pancreatitis requiring pancreatectomy. It is less invasive with lower morbidity than pancreas transplantation and can alleviate requirements of insulin therapy. The primary advantage of this cell-based therapy over conventional insulin therapy is that islets can provide a more naturally balanced hormonal response to physiological nutrient and energy levels to moderate blood glucose and reduce glycosylated hemoglobin (HbA1C) without eliciting dangerous levels of hypoglycemia. Indeed, transplanted islets can reduce or prevent hypoglycemic episodes in cases of individuals requiring insulin therapy with hypoglycemic unawareness or brittle diabetes. Thus, islet transplantation not only provides a means to regulate blood glucose by replacing islet cells harboring natural responses to physiological stimuli, but is also an important therapeutic option for patients unable to sense hypoglycemia with increased risk of health and lifestyle complications from unstable fluctuations in blood glucose.
One of the major challenges of islet transplantation is long-term survival and function of the islet graft. Although significant improvements to procedures over the last couple of decades have increased success rates to achieve insulin independence, the rates significantly decline within 1-3 years after transplantation. Islets are subjected to damage and stress throughout transplantation procedures and there is attrition of islet mass and function following engraftment. This is largely attributed to inflammatory and an acute innate immune response. This early immune response is mediated in part by platelet and complement components of the blood that interact with the islet. The phenomenon has been referred to as the Instant Blood Mediated Inflammatory Reaction (IBMIR). As the blood reacts with the infused digested and exposed islet tissue, monocytes are recruited to the site to evoke an immune response. However, blood components and immune cells do not act alone in this process. The islet cells themselves produce chemokines and cytokines that exacerbate the response. We have referred to these islet cell cytokines as “isletokines” to distinguish their origin from immune cells. Stressed islets produce and release isletokines that can recruit immune cells to the graft and evoke a vicious cycle of immune reactivity (Figure 1). Thus, strategies for interfering with production of isletokines from islets and their communication with immune cells could potentially break the cycle of islet-immune cell interactions that exacerbate inflammatory damage and promote further downstream immune destruction of the islet graft. In this review, we discuss current pharmacological targets that have advanced immunosuppression regimens during islet transplantation and follow up with the novel strategies for targeting components of the acute innate response during the early post-transplant period that may reduce requirements of immunosuppression and preserve long-term islet cell mass and function.
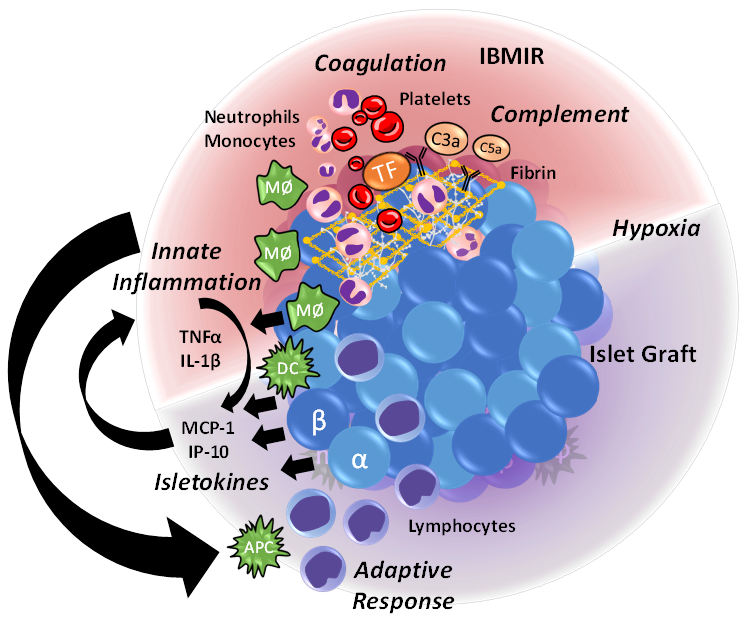
Figure 1 Factors contributing to acute islet inflammation and cyclical amplification of islet-immune cell reactivity. The acute inflammatory reaction highlighted in red consists of a thrombotic “IBMIR” response when isolated and damaged islet tissue is exposed to blood and initiates coagulation and complement cascades. Tissue factor (TF) produced by damaged islets promotes the coagulation by attracting platelets and leukocytes to produce a fibrin clot that contributes to islet hypoxia. Stressed islets release cytokines that recruit and activate neutrophils, macrophages (MΦ), and dendritic cells (DC) to the grafting site. Infiltrating and activated immune cells further promote islet inflammation and production of antigen-presenting cells (APC) that activate lymphocytes and induce an adaptive response. These cyclical and amplifying factors contribute to islet-immune cell mediated graft failure.
2. Inhibition of Calcineurin and mTOR for Global Immune Suppression
To date, the FK506 immunophilin binding protein macrolides, FK506 (tacrolimus) and rapamycin (sirolimus) have remained cornerstone compounds for lymphocytic immunosuppression in modern allotransplantation [1,2,3,4,5,6,7]. This is largely attributed to their potent pharmacological inhibition of intracellular signaling targets that induce lymphocyte activation and proliferation, respectively. Tacrolimus inhibits calcineurin, which in turn regulates the nuclear factor of activated T cells (NFAT) transcription factor required for T cell receptor (TCR) induction of key cytokines and receptors that mediate T cell activation. Sirolimus inhibits the mammalian target of rapamycin (mTOR) serine/threonine kinase complex 1 (mTORC1) which is part of the PI3K-AKT signaling arm required for lymphocyte cell proliferation and differentiation in response to cytokines. Thus, both tacrolimus and rapamycin can complement each other in synergistic effects of 1) suppressing cytokine expression and 2) preventing cytokine action on T and B cell expansion, respectively.
However, just as in the case with other allotransplant procedures, immunosuppression regimens involving long-term use of tacrolimus or rapamycin to protect islet graft mass and function come with increased risk of morbidity. The major clinical drawbacks of calcineurin and mTOR inhibition (CNI and mTORI) include significant side effects of nephrotoxicity, islet toxicity, and increased risk of infection resulting from global immunosuppression. As such, there has been intense interest in identifying equipotent alternatives to reduce significant long-term side effects observed from prolonged use of CNI and mTORI. Several approaches to avoiding or minimizing toxicities have been utilized and have had considerable success in utilizing lower doses of CNI or mTORI in combination with other less potent, but also less toxic immunosuppressants.
3. Selective Inhibition of Lymphocytes to Prolong Islet Graft Survival
3a) Mycophenolate mofetil (MMF), a prodrug morpholinoethyl ester of active compound mycophenolic acid (MPA), for example, has revealed a unique pathway for suppressing lymphocytes in allogeneic rejection [8,9] Its prime mechanism of action is to inhibit the intracellular enzyme inosine monophosphate dehydrogenase and deplete guanine nucleotide de novo synthesis. This, in turn, selectively suppresses phosphoribosyl pyrophosphate synthetase and DNA polymerase activity in lymphocytes, which is required for DNA replication and cellular proliferative responses to mitogenic stimuli [10]. Although not potent enough to provide adequate immunosuppression to prevent rejection alone, MMF has been successfully substituted for either tacrolimus or sirolimus in maintenance therapy withdrawal protocols to reverse nephrotoxicity and improve islet function [11,12]. These studies suggest that immunomodulation of events occurring in the early post-transplant period can subsequently reduce side effects associated with tacrolimus based long-term immunosuppression.
Major improvements in islet transplantation success rates have also come from advances in immunosuppression protocols involving antibody induction therapies in conjunction with maintenance therapy drugs to prevent lymphocyte activation and proliferation. This has primarily been achieved through selectively targeting lymphocyte surface receptors.
3b) Induction by monoclonal antibody daclizumab which binds to the CD25 alpha subunit of the IL-2 receptor on T cells helped provide landmark improvements in islet transplant outcomes when introduced with the Edmonton Protocol in 2000 [13]. Due to safety concerns of daclizumab, other lymphocyte receptor targets have been explored and have led to promising improvements in immunosuppressant regimens to extend islet graft survival with reduced toxicities [14].
3c) Anti-CD3 monoclonal antibodies (hOKT3γ1 Ala-Ala) or polyclonal anti-thymocyte immunoglobulin antibody preparation (thymoglobulin) to prevent expansion or deplete circulating effector T cells have extended islet graft survival with reduced requirements of tacrolimus or sirolimus [14].
3d) Alemtuzumab (Campath and Lemtrada), a humanized IgG1 monoclonal anti-CD52 antibody used to treat chronic lymphocytic leukemia and multiple sclerosis, has been observed to improve islet engraftment and rates of insulin-independence with improved tolerance [15]. Multiple mechanisms have been proposed for actions of alemtuzumab including antibody-dependent cell-mediated (ADCC) and complement-dependent (CDC) cytotoxicity toward T cells and B cells with high expression of glycosylphosphatidylinositol-linked surface protein CD52. It has sparing effects toward immature lymphocytes and innate immune cells having relatively low CD52 expression and preserves regulatory T cells that may contribute to graft survival [14,16,17]. Indeed, alemtuzumab treatment in a humanized mouse model showed that natural killer cells and neutrophils contribute to lymphocyte depletion independently of CDC. These studies suggest that the innate immune system also has a role in regulating the adaptive response under these conditions [18].
3e) Efalizumab, another humanized monoclonal antibody that targets the CD11a subunit of the leukocyte function antigen (LFA-1) showed promising results to prolong islet cell survival in single donor islet transplants without side effects observed by standard long-term tacrolimus and sirolimus [19]. Its unique action is to prevent binding of LFA-1 to intercellular adhesion molecule (ICAM) required for leukocyte extravasation to provide immunosuppression without T cell depletion. Unfortunately, long-term use of efalizumab for more than 4 years was associated with increased risk (~1 in 10,000) for progressive multifocal leukoencephalopathy (PML) in psoriasis patients, which led to its voluntary withdrawal from the global market by its sponsor. This consequently led to the finding that abatacept, the CD80 targeting CTLA-4 human Fc IgG1 fragment linked fusion protein, could sustain graft survival in islet transplant patients as a replacement for efalizumab when it was withdrawn from protocols during clinical trials.
3f) Belatacept, a second generation CTLA-4 fusion protein product with enhanced affinity toward both CD80 and CD86, could also provide insulin-independence when co-administered with sirolimus as a substitute for tacrolimus after thymoglobulin induction [20,21]. These CTLA-4 fusion proteins bind to CD80/CD86 and interfere with co-stimulatory requirements of APC antigens binding to CD28 to activate T cells. These clinical findings define yet another set of lymphocyte surface receptors that can be selectively targeted in CNI-sparing immunosuppressant regimens.
Collectively, these observations demonstrate that 1) multiple cell surface receptors can be effectively targeted on lymphocytes to prolong graft survival and 2) individual components of lymphocyte signaling can be selectively targeted to substantially inhibit lymphocyte activation and expansion. However, even when lymphocytes are selectively inhibited or depleted in the absence of tacrolimus or sirolimus, rejection still occurs. This suggests that lymphocyte inhibition alone is not sufficient to prevent alloimmune rejection and that other cellular mechanisms contribute to loss of islet graft mass and function. Indeed, components of innate immunity have been characterized to regulate the adaptive response in allo- and auto-immunity.
4. Non-Lymphocyte Cell Mediated Loss of Islet Graft Mass and Function
Mounting evidence indicates that innate immune cells not only initiate adaptive immune responses, but also directly contribute to allograft rejection [22,23,24,25]. Perhaps this is most evident in autologous islet transplantation where a large portion of the graft is lost in the absence of a T-cell mediated response [26]. Indeed, more than 50% of the islet graft is lost due to an acute innate response [27,28,29,30]. The initial islet cell mass is a key determinant of clinical islet transplant outcomes. Thus, the early post-transplant period during which an acute innate response occurs represents an important window of opportunity to extend the life of the graft.
Moreover, targeting innate immune cells may also alleviate subsequent priming or exacerbation of adaptive immune responses toward transplanted islets. Cells contributing to the acute innate response include platelets, neutrophils, macrophages, dendritic cells (DCs), natural killer (NK) cells and the islet endocrine cells themselves. Both cellular and humoral components, part of which have been described as IBMIR, produce coagulation and complement activation to produce an inflammatory environment that destroys up to half the graft before lymphocytes ever make it to the scene. Therefore, targeting acute islet inflammation in conjunction with lymphocyte alloimmune and autoimmune suppression must be taken into consideration when devising novel strategies to achieve highest islet transplant success rates.
In the following, we first reevaluate what is currently known about the mechanistic contributions of innate immunity to adaptive alloimmune responses in transplantation. In addition, we discuss potential targets based on recent and ongoing studies in animal models and clinical trials that may further advance our methods to improve clinical islet transplant outcomes.
4.1 Regulation of the Adaptive Response by Innate Immune Cells
The founding concept that the innate immune system could sense non-self antigens by receptors was first introduced by Charles Janeway, Jr. who proposed that pattern recognition receptors (PRRs) recognize bacterial or viral molecules termed pathogen-associated molecular patterns (PAMPs) [31,32,33]. Innate immune recognition toward conserved components of microbial non-self antigens induced expression of co-stimulatory molecules to activate lymphocytes with reactivity toward the presented antigen. However, this model did not adequately describe how innate immunity could confer adaptive responses toward non-self tissue allografts and tumors or reactivity toward self antigens in autoimmune diseases in the absence of microbes in an otherwise “sterile” environment. Thus, the concept was further developed by Polly Matzinger who later introduced the “danger hypothesis” to describe innate immune cells recognizing self-antigen molecules from stressed or damaged cells as an associated danger and subsequently activating defenses and repair mechanisms [34,35,36].
This broad array of molecules was referred to as danger associated molecular patterns (DAMPs) which include reactive oxygen species (ROS), ATP, uric acid crystals, high mobility group protein b1 (HMGB1), nucleic acids, fibronectin, hyaluronic acid, and heparan sulfate among many others. DAMPs are recognized by a diverse set of PRRs including Toll like receptors (TLR) and IL-1 receptor (IL-1R) of the Toll/IL-1R (TIR) superfamily to initiate signaling pathways that induce an inflammatory response in stressed or damaged tissue. Upon binding to DAMPs, TLR and IL-1R recruit myeloid differentiation primary response 88 (MyD88) adapter protein and IL-1R-associated kinase (IRAK) family kinases to form a receptor complex that activates E3 ubiquitin ligases TRAF6 and Pellinos. This results in formation of Lys63- and Met1- linked ubiquitin chain co-recruitment of TAK1 and canonical IκB kinase (IKK) master kinase complexes, respectively. TAK1 activates MAP kinase kinase (MKK) cascades that switch on p38 and c-Jun N terminal kinase (JNK) MAP kinases while the IKKβ component of IKK activates the nuclear factor kappa-light chain-enhancer of activated B cells (NF-κB) transcription factor. MAP kinases and NF-κB coordinately regulate several cytokine and chemokine genes that induce proliferation and mediate inflammation at the site of damage.
As innate immune cells are recruited to the site of inflammation, more cytokines and chemokines are produced to activate and recruit cells required to repair and regenerate damaged tissue. Overstimulation or chronic activation of inflammatory signaling pathways in target cells results in ER stress and can induce apoptosis and cell death. If damage signals are not appropriately resolved or the tissue cannot be restored to a normal non-stressed physiological state, innate immune cells proceed to destroy and phagocytose tissue at the site. Immune cells then circulate back to lymphoid cells for antigen presentation and acquire memory for further targeted destruction of the recalcitrant threat. In this way, the innate immune system activates and tailors the adaptive response toward dangerous conditions or invasive cells that may threaten homeostasis or the physiological integrity of the host.
4.2 DAMP Signaling and IBMIR in Acute Islet Inflammation
In the case of islet transplantation, the graft is subjected to damage and insults that produce DAMPs during multiple steps throughout the transplantation process. DAMPs are already being produced and released by stressed and damaged tissue in cadaveric donors due to traumas related to brain death or by ischemia and organ recovery in the case of live tissue donors. In addition, virtually all graft tissue undergoes some forms of stress insults and damage during procurement and transport. These include temperature changes, ROS, hypoxia, and ischemia-reperfusion injury. During the islet isolation process, the pancreas is also subjected to enzymatical digestion, hypoxia, and mechanical stress [37]. This further produces DAMPs that can directly induce production and release of inflammatory cytokines by activating TLRs on both innate immune cells and islet endocrine cells ex vivo. These cytokines accumulate with DAMPs in a vicious cycle over the duration of the isolation process and are reintroduced into the recipient host at the time of islet infusion.
The combination of DAMPS, cytokines, and blood components interacting with islet tissue proteins and receptors upon infusion culminate into an acute thrombotic reaction known in the field of islet transplantation as IBMIR. Bennet and colleagues first described this event by characterizing cellular interactions between freshly isolated human islets and ABO compatible allogeneic blood [38]. Engagement of IgG and IgM antibodies with islet cell surface collagen and laminins play a key role in initiating the complement cascade. In parallel, the glycoprotein CD142 tissue factor, expressed on the cell surface and released by damaged and stressed islets, binds to factor VII to catalyze the coagulation cascade [39,40,41,42]. Platelets activated during this process produce a fibrin mesh clot surrounding the islets resulting in their embolic occlusion within the hepatic sinusoids of the liver [43,44]. This in turn deprives the graft of oxygen and nutrients leading to increased apoptosis and necrosis further contributing to increased DAMPs, proinflammatory cytokines, and immune cell infiltration.
4.3 Islet Contributions to Acute Graft Inflammation
In addition to expressing proteins that interact with blood components to initiate complement and coagulation cascades, islets express isletokines that contribute to initiating and exacerbating acute inflammation. Several cytokines have been identified in islets during diabetes and in islet grafts [45,46]. Originally, it was assumed that infiltrating immune cells were sole producers of proinflammatory cytokines in islets. However, flow cytometry, immunohistochemistry, and laser capture analysis studies revealed that the islet endocrine cells also produce proinflammatory mediators that can elicit immune cell responses [47,48,49,50,51,52,53,54,55]. In fact, the islet cells produce and release dozens of isletokines that can be detected in the blood circulation upon infusion that correlate with transplant outcomes [55,56]. In particular, HMGB1, MCP-1 and IP-10 are highly expressed and released in damaged or stressed islets and play a key role in initiating acute inflammation in transplanted islets [55,57,58,59,60,61,62].
Induction of isletokine genes in the endocrine component of islet cells is conferred by DAMP and cytokine-induced signaling. In pancreatic beta cells, DAMPs can activate TLR/IL-1R signaling to induce activation of MAP kinases and NF-κB. In addition, CN and NFAT signaling can be activated by TLR/IL-1R [63]. The culmination of MAP kinases and NF-κB and NFAT signaling results in the induction of multiple cytokine genes in beta cells, including IL-1β, TNF-α, HMGB1 and IP-10. IL-1β and TNF-α can further stimulate NF-κB- and NFAT-mediated isletokine gene expression in beta cells. Moreover, HMGB1 and IP-10 not only function as chemokines to recruit immune cells, but also act as DAMPs which can bind to and activate TLR4 [64]. Thus, DAMP and cytokine-induced signaling can produce a vicious cycle of damage and inflammation if not resolved by damage-repair mechanisms. In the case of islet transplantation, the islet cells are stripped of their natural niche within the pancreas and exposed to a new location in a damaged state. Sustained expression and release of isletokines by beta cells out of their natural context results in amplified proinflammatory and adaptive immune responses contributing to graft destruction (Figure 1).
4.4 Hypoxia and Oxidative Stress in Islets
Pancreatic beta cells are enriched with GLUT2 glucose transporters, allowing them to dynamically uptake and utilize glucose in the blood as one of the most metabolically active tissues [65]. Oxygen is required to maintain beta-cell function through the tricarboxylic acid (TCA) cycle, which links synthesis of intracellular ATP to the production and release of insulin [66]. ROS generated through production of ATP by the TCA cycle also contribute to signaling mechanisms that regulate glucose-induced insulin secretion [67,68]. Thus, a sensitive and carefully balanced redox system allows beta cells to sense nutrient load and appropriately produce insulin upon physiological demand. This is achieved in part by a significantly lower expression of ROS-depleting enzymes superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx) in beta cells compared to other tissues. These inherent characteristics of metabolic sensing make beta cells particularly vulnerable to redox imbalance and oxidative stress [67,69,70,71].
Extreme conditions of oxygen availability, oxygen consumption, and metabolic stress can offset redox balance and result in oxidative stress. Chronic exposure of beta cells to high glucose and increased metabolic flux favors mishandling of excess electrons via NADH and FADH2 and the mitochondrial electron transport chain, which transfer and reduce O2 to superoxide free radicals and further generate ROS [71]. In the absence of appropriate oxygen tension, i.e. hypoxia, NADH and FADH2 can also accumulate with inefficient aerobic respiration, allowing electrons to escape and produce excessive ROS [71]. Uncontrolled generation of ROS disrupts redox signaling and leads to oxidative damage of cellular proteins, lipids, and DNA [72,73].
The hepatic portal system site of transplantation offers lower parenchymal oxygen tension and vasculature compared to pancreatic portal system. At lower cellular oxygen concentrations, prolyl-4-hydroxylases (PHDs) are inhibited which consequently allows increased expression and activation of hypoxia-inducible factor-1 alpha (HIF-1α) and NF-κB [74,75,76,77]. These transcription factors acutely regulate genes involved in hypoxic and metabolic adaptation. However, they concomitantly also induce cytokines that induce inflammation [78,79]. Cytokines can contribute to ER stress, nitric oxide (NO) and ROS generation to further activate NF-κB, p38 and JNK MAP kinase pathways that regulate uncoupled protein response and inflammatory genes [80,81,82]. When hypoxic and inflammatory stress are sustained, these pathways activate apoptotic programming [83,84]. Thus, hypoxia can induce and exacerbate conditions of oxidative and inflammatory stress in islets by overlapping pathways leading to immune destruction and beta-cell death.
5. Strategies to Prevent Islet-Immune Cell Mediated Loss of Islet Graft Mass and Function
Attempts to inhibit immune cell function by pharmacological agents have provided invaluable information regarding requirements and specificity of molecular targets for induction of immune responses to allografts. For example, selective inhibition of intracellular targets CN and mTOR have shown most potent effects to prevent alloimmune rejection. Their mode of action is primarily attributed to suppression of cytokine production and responses in lymphokines, respectively. However, accumulating evidence indicates that blocking these intracellular targets is not specific to lymphocyte cell types and that CN and mTOR also regulate cytokines in innate immune cells and islet endocrine cells [54,85,86,87,88]. This is further complicated by the findings that islets require CN and mTOR pathways for physiological adaptation and cellular function [89,90,91,92].
Because most intracellular signaling pathways are shared among multiple immune and non-immune cell types with diverse functions, their inhibition often results in adverse off-target effects. Indeed, sustained blockade of CN and mTOR contributes to side effects beyond immunosuppression, most notably damage to kidney and islet cell function. Moreover, CN/NFAT signaling has been shown to have a role in limiting DC priming of T cells and regulating Treg-mediated immune tolerance [93,94]. mTOR also regulates cytokine production in myeloid cells in response to TLR signaling and induces tolerogenic DC phenotypes [95]. Thus, although CN and mTOR inhibition has potent effects to break islet-immune cell interactions by modulating cytokine signaling in beta cells and lymphocytes, the benefits are offset by toxicity to other tissue functions and impairment of immune tolerance. This prompted the field to explore alternative, more cell-selective targets for immune suppression.
As new molecular targets have been identified that are uniquely expressed by subsets of cells, novel pharmaceutical approaches have been pursued that selectively effect cell-specific mechanisms involved in pathogenic processes. As reviewed above, several monoclonal antibodies and soluble mediators have been successful in meeting these criteria by targeting unique surface molecules or receptor-mediated cell signaling. Although there have been considerably less side effects in several trial regimens focusing on select targets of inflammation and immune responses, it is becoming increasingly clear that there are multiple components throughout transplant procedures that need to be targeted to prolong graft survival. The key components include 1) the lymphocytic response that directly erodes islet cell mass and function, 2) the acute inflammatory response that destroys a large portion of the graft during the early peri-transplant period, and 3) cytokine signaling between the islets and immune cells that perpetuate and amplify innate and adaptive immune responses.
First and foremost, resetting auto- and alloimmune reactivity by T cell and B cell depletion induction therapy in the host/recipient appears to be a prerequisite to achieving long-term allograft survival and function [14]. Thymoglobulin and alemtuzumab induction has been shown to have beneficial effects in reducing the rate of acute rejection when combined with maintenance regimens. MMF and belatacept have thus far been most promising in helping maintain suppressed immune reactivity after lymphocyte depletion with reduced side effects attributed to CNI and mTORI. However, MMF and belatacept only delay loss of allograft function, and rejection is accelerated in the absence of tacrolimus or sirolimus.
The next important step to improving islet transplantation is to selectively reduce the acute innate inflammatory response in islets occurring during the early transplant period. Benefits in graft survival and function have been observed from combinatorial approaches of lymphocyte depletion and anti-inflammatory soluble mediators etanercept and anakinra to block TNF-α and IL-1β signaling, respectively. These clinical findings indicate that early blockade of key cytokines during the induction period can improve long-term clinical outcomes. Double blockade by both etanercept and anakinra improves the response [96]. There is also strong evidence to suggest that chemokines MCP-1 and IP-10 play key roles in initiating inflammatory responses in islet transplantation [55,57]. It should also be noted that IP-10 is a key isletokine expressed by beta cells in insulitic lesions in type 1 diabetes [97,98,99]. The use of anti-IP-10 neutralization antibody after T-cell depletion by anti-CD3 antibody prevented reinfiltration of islet-specific T cells and resulted in remission of diabetes [100]. Based on these observations, it is conceivable that a combinatorial approach to resetting the adaptive response by lymphocyte depletion and neutralizing key isletokines, which evoke islet inflammation, could break the cycle of innate immune activation of adaptive responses toward islets.
Interestingly, transgenic animal studies show that whereas islet donor-derived IP-10 induces graft-damaging inflammation upon transplantation, islet donor-derived MCP-1 is not required for graft failure [101]. Detrimental effects on donor islets were only observed when MCP-1 production was intact in graft recipients and IP-10 was intact in donor islets. In either case, blocking MCP-1 or IP-10 signaling reduced islet inflammation and anti-IP-10 neutralizing monoclonal antibody prolonged graft survival. Together, these studies indicate that graft damage observed by MCP-1 is propagated by the recipient immune system in response to donor-selective IP-10-induced inflammation. They also provide proof of concept that blocking IP-10-induced inflammation by a monoclonal antibody could prevent early loss of islet grafts and improve islet transplant outcomes. Further study needs to be performed to determine if a trio of soluble mediators targeting TNF-α, IL-1β, and IP-10 could provide additional benefit for blocking the acute innate inflammatory response to warrant its use in clinical islet transplantation.
To achieve highest efficacy in targeting acute islet inflammation, it must also be recognized that inflammatory events are already occurring in donor islets prior to infusion, beginning as early as donor trauma and organ procurement. Thus, approaches to alleviate inflammatory stress could be implemented as early as time of procurement and throughout the islet isolation process during which islets are stressed and producing proinflammatory isletokines. These isletokines are released at their highest level upon islet infusion and remain high during the IBMIR response. Thus, the early procedures of the islet cell transplant process are potential key target areas for suppressing acute inflammation and preventing large losses of islet cell mass.
Strategies for complete protection of islets from the acute inflammatory response will require further upstream procedural approaches to include therapeutic interventions in isolation of the recipient. These pre-transplant interventions would allow blockade of intracellular stress response signals and could be performed ex vivo with minimal exposure of pharmacological agents to the host. For example, efforts to block CN/NFAT signaling or other cellular targets required for cytokine production could be performed during organ procurement and islet isolation procedures ex vivo without adverse effects associated with recipient long-term systemic use.
Although there are multiple reports indicating direct effects of CNI to inhibit beta cell proliferation, insulin transcription, and GSIS, we and others have shown it to have minimal effects on beta cell viability and apoptosis within short durations of in vitro exposure [102,103]. Moreover, short-term administration of tacrolimus has been shown to have no effect on islet secretion in healthy human subjects and improves beta cell viability and function when islets are under stress [102,104,105]. Indeed, acute exposure of tacrolimus prevents apoptosis in islets exposed to cytokines in vitro and can restore insulin gene transcription in islets chronically exposed to high glucose within a 48 h window [106,107]. Furthermore, short-term peptide inhibition of the CN downstream target NFAT in islets was shown to prolong graft function in an allogeneic mouse transplant model. Thus, the use of tacrolimus during pre-transplant and induction procedures may provide benefits to inhibit the acute innate response, thereby reducing its requirements for maintenance therapy.
Benefits of inhibition of TLR/IL-1R and downstream activation of NF-κB and p38 and JNK MAP kinase signaling pathways to reduce cytokine production and apoptosis in islets in vivo have also been observed [108,109,110,111,112,113]. Ex-vivo surface modification of islets with a slow-releasing TLR4-selective antagonist TAK242 improved islet graft survival in a syngeneic mouse model. Moreover, the use of TAK242 during pancreatic ductal perfusion and digestion steps of the islet isolation process reduced activation of MAPK stress kinase signaling and expression of proinflammatory cytokines to prolong islet viability and function. TLR4 is one of several mechanisms to activating MAPKs and NF-kB in islets and other targets should be explored during pre-transplantation procedures. For example, it would be predicted that blockade of IL-1R signaling by anakinra in addition to TLR blockade during these steps would further prevent cytokine and DAMP-mediated inflammatory reactions in islets.
TLR activation not only augments the acute innate response, but contributes to the adaptive immune response through effects on antigen-presenting cells (APCs) and activation of T cells [114,115,116]. In APCs, TLRs drive maturation as well as production of IL-12 that results in T helper cells (Th1) response [114]. MyD88 dependent TLR signaling inhibition resulted in reduced numbers of activated CD4+ and CD8+ T cells and increased mortality rates of mice [117]. TLR-knockout murine models are evidence of the initiation and development of an adaptive host resistance to pathogens that is dependent on the TLR/IL-1R activation of MyD88 signaling pathways described above [114,118,119]. Most notably, TLR-stimulated islets were shown to induce islet graft failure by a CD8+ T cell-dependent mechanism [115]. These findings indicate that selective inhibition of TLR signaling in islets could potentially alleviate or prolong onset of lymphocyte-mediated destruction of the islet graft.
Lastly, anticoagulants have been shown to reduce the acute inflammatory response [120]. This is evident from reports on inhibition of thrombin by melagatran or heparin in vitro [38,121]. Despite routine use of systemic heparin in the clinical setting, the formation of micro and macrothrombi is not completely blocked, leading to the observed loss of islet graft mass in the days immediately after transplantation. Interestingly, short-term administration of acute phase reactant serine protease inhibitor alpha 1-antitrypsin (AAT) could dramatically improve survival of human, monkey, and mouse islet grafts in animal models [122,123]. This was attributed to suppression of blood-mediated coagulation pathways, inhibition of NF-κB signaling, downregulation of inflammatory mediators, and reduced CD3+ T cells and F4/80+ activated monocytes in grafted islets. These findings indicate that AAT has useful properties for both anti-coagulation and anti-inflammatory therapies in islet transplantation. Multiple clinical trials are investigating the effects of AAT ARALAST NP during islet processing, culture, and patient treatment pre- and post- transplant on the acute inflammatory response in both allogeneic and autologous islet transplantation.
6. Conclusions
Islet cell destruction during transplantation results from complex cell signaling communication between islet cells and immune cells, linking islet inflammatory stress responses to innate and adaptive immune responses. Damaged and stressed islets release inflammatory mediators that recruit and activate immune cells, which attempt to resolve or remove damaged, foreign, or maladaptive tissue. Delinking this process can break an amplifying cycle of inflammation and immune sensitization toward transplanted islets. Because an acute innate inflammatory response largely affects islet graft mass and dictates further downstream adaptive immune events, it follows that early intervention of islet-immune cell interactions may be key to improving islet transplant outcomes. Hence, the most successful islet transplant regimens going forward will likely be interventions targeting both islet-induced inflammation and activation of innate immune cells in addition to T-cell mediated immune events.
Author Contributions
CMD and MCL contributed to manuscript writing and figure design; SV, KK, and BN contributed feedback, proofreading, and editing for the manuscript.
Competing Interests
The authors have declared that no competing interests exist.
References
- Kino T, Hatanaka H, Hashimoto M, Nishiyama M, Goto T, Okuhara M, et al. FK-506, a novel immunosuppressant isolated from a streptomyces. J Antibiot. 1987; 40: 1249-1255. [CrossRef]
- Morris PJ. Cyclosporine, FK506 and other drugs in organ transplantation. Curr Opin Immunol. 1991; 3: 748-751. [CrossRef]
- Bierer BE, Holländer G, Fruman D, Burakoff SJ. Cyclosporin A and FK506: Molecular mechanisms of immunosuppression and probes for transplantation biology. Curr Opin Immunol. 1993; 5: 763-773. [CrossRef]
- Thomson AW, Starzl TE. New immunosuppressive drugs: Mechanistic insights and potential therapeutic advances. Immunol Rev. 1993; 136: 71-98. [CrossRef]
- U.S. Multicenter FK506 liver study group. A comparison of tacrolimus (FK 506) and cyclosporine for immunosuppression in liver transplantation. N Engl J Med. 1994; 331: 1110-1115. [CrossRef]
- Laskow DA, Neylan JF, Shapiro RS, Pirsch JD, Vergne-Marini PJ, Tomlanovich SJ. The role of tacrolimus in adult kidney transplantation: a review. Clin Transplant. 1998; 12: 489-503.
- Azzi JR, Sayegh MH, Mallat SG. Calcineurin inhibitors: 40 years later, can’t live without .. J Immunol. 2013; 191: 5785-5791. [CrossRef]
- Sollinger HW, Belzer FO, Deierhoi MH, Diethelm AG, Gonwa TA, Kauffman RS, et al. RS-61443 (mycophenolate mofetil). A multicenter study for refractory kidney transplant rejection. Ann Surg. 1992; 216: 513-519. [CrossRef]
- Sollinger HW. Mycophenolate mofetil for the prevention of acute rejection in primary cadaveric renal allograft recipients. U.S. Renal Transplant Mycophenolate Mofetil Study Group. Transplantation. 1995; 60: 225-232. [CrossRef]
- Allison AC, Eugui EM. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology. 2000; 47: 85-118. [CrossRef]
- Senior PA, Paty BW, Cockfield SM, Ryan EA, Shapiro AMJ. Proteinuria developing after clinical islet transplantation resolves with sirolimus withdrawal and increased tacrolimus dosing. Am J Transplant. 2005; 5: 2318-2323. [CrossRef]
- Froud T, Baidal DA, Ponte G, Ferreira JV, Ricordi C, Alejandro R. Resolution of neurotoxicity and beta-cell toxicity in an islet transplant recipient following substitution of tacrolimus with MMF. Cell Transplant. 2006; 15: 613-620. [CrossRef]
- Shapiro AM, Lakey JR, Ryan EA, Korbutt GS, Toth E, Warnock GL, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000; 343: 230-238. [CrossRef]
- Bellin MD, Barton FB, Heitman A, Alejandro R, Hering BJ. Potent induction immunotherapy promotes long-term insulin independence after islet transplantation in type 1 diabetes. Am J Transplant. 2012; 12: 1576-1583. [CrossRef]
- Froud T, Baidal D, Faradji R, Cure P, Mineo D, Selvaggi G, et al. Islet transplantation with alemtuzumab induction and calcineurin-free maintenance immunosuppression results in improved short and long-term outcomes. Transplantation. 2008; 86: 1695-1701. [CrossRef]
- Toh B-H, Kyaw T, Tipping P, Bobik A. Immune regulation by CD52-expressing CD4 T cells. Cell Mol Immunol. 2013; 10: 379-382. [CrossRef]
- Simon M, Ipek R, Homola GA, Rovituso DM, Schampel A, Kleinschnitz C, et al. Anti-CD52 antibody treatment depletes B cell aggregates in the central nervous system in a mouse model of multiple sclerosis. J Neuroinflammation. 2018; 15: 225. [CrossRef]
- Hu Y, Turner MJ, Shields J, Gale MS, Hutto E, Roberts BL, et al. Investigation of the mechanism of action of alemtuzumab in a human CD52 transgenic mouse model. Immunology. 2009; 128: 260-270. [CrossRef]
- Turgeon N, Avila J, Cano J, Hutchinson J, Badell I, Page A, et al. Experience with a novel efalizumab-based immunosuppressive regimen to facilitate single donor islet cell transplantation. Am J Transplant. 2010; 10: 2082-2091. [CrossRef]
- Posselt AM, Szot GL, Frassetto LA, Masharani U, Tavakol M, Amin R, et al. Islet transplantation in type 1 diabetic patients using calcineurin inhibitor-free immunosuppressive protocols based on T-cell adhesion or costimulation blockade. Transplantation. 2010; 90: 1595-1601. [CrossRef]
- Gardner JM, Posselt AM, Wisel S, Mashirani U, Szot G, Nguyen V, et al. Ten year insulin-independence in select islet transplant recipients receiving CNI-sparing immunosuppression with either costimulation blockade or anti-LFA1. Transplantation. 2018; 102: S374. [CrossRef]
- McNerney ME, Lee KM, Zhou P, Molinero L, Mashayekhi M, Guzior D, et al. Role of natural killer cell subsets in cardiac allograft rejection. Am J Transplant. 2006; 6: 505-513. [CrossRef]
- Maier S, Tertilt C, Chambron N, Gerauer K, Hüser N, Heidecke CD, et al. Inhibition of natural killer cells results in acceptance of cardiac allografts in CD28-/- mice. Nat Med. 2001; 7: 557-562. [CrossRef]
- Obara H, Nagasaki K, Hsieh CL, Ogura Y, Esquivel CO, Martinez OM, et al. IFN-γ, produced by NK cells that infiltrate liver allografts early after transplantation, links the innate and adaptive immune responses. Am J Transplant. 2005; 5: 2094-2103. [CrossRef]
- Kirk AD, Hale DA, Mannon RB, Kleiner DE, Hoffmann SC, Kampen RL, et al. Results from a human renal allograft tolerance trial evaluating the humanized CD52-specific monoclonal antibody alemtuzumab (CAMPATH-1H). Transplantation. 2003; 76: 120-129. [CrossRef]
- Chu X, Kilpatrick E, Xiao X, Liu W, Demirci G, Exley M, et al. Islet allograft tolerance in the absence of invariant natural killer T cells. Clin Immunol. 2011; 141: 268-272. [CrossRef]
- Saudek F, Jirák D, Girman P, Herynek V, Dezortová M, Kríž J, et al. Magnetic resonance imaging of pancreatic islets transplanted into the liver in humans. Transplantation. 2010; 90: 1602. [CrossRef]
- Eich T, Eriksson O, Sundin A, Estrada S, Brandhorst D, Brandhorst H, et al. Positron emission tomography: a real-time tool to quantify early islet engraftment in a preclinical large animal model. Transplantation. 2007; 84: 893-898. [CrossRef]
- Eich T, Eriksson O, Lundgren T. Visualization of early engraftment in clinical islet transplantation by positron-emission tomography. New Engl Med. 2007; 356: 2754-2755. [CrossRef]
- Malosio ML, Esposito A, Brigatti C, Palmisano A, Piemonti L, Nano R, et al. MR imaging monitoring of iron-labeled pancreatic islets in a small series of patients: Islet fate in successful, unsuccessful, and autotransplantation. Cell Transplant. 2015; 24: 2285-2296. [CrossRef]
- Janeway CA. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harb Symp Quant Biol. 1989; 54: 1-13. [CrossRef]
- Medzhitov R, Janeway CA. Innate immunity: The virtues of a nonclonal system of recognition. Cell. 1997; 91: 295-298. [CrossRef]
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006; 124: 783-801. [CrossRef]
- Matzinger P. Tolerance, danger, and the extended family. Annu Rev Immunol. 1994; 12: 991-1045. [CrossRef]
- Matzinger P. The danger model: A renewed sense of self. Science. 2002; 296: 301-305. [CrossRef]
- Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: Endogenous activators of dendritic cells. Nat Med. 1999; 5: 1249-1255. [CrossRef]
- Bottino R, Balamurugan AN, Tse H, Thirunavukkarasu C, Ge X, Profozich J, et al. Response of human islets to isolation stress and the effect of antioxidant treatment. Diabetes. 2004; 53: 2559-2568. [CrossRef]
- Bennet W, Sundberg B, Groth CG, Brendel MD, Brandhorst D, Brandhorst H, et al. Incompatibility between human blood and isolated islets of Langerhans: a finding with implications for clinical intraportal islet transplantation? Diabetes. 1999; 48: 1907-1914. [CrossRef]
- Tjernberg J, Ekdahl KN, Lambris JD, Korsgren O, Nilsson B. Acute antibody-mediated complement activation mediates lysis of pancreatic islets cells and may cause tissue loss in clinical islet transplantation. Transplantation. 2008; 85: 1193-1199. [CrossRef]
- Nilsson B, Ekdahl KN, Korsgren O. Control of instant blood-mediated inflammatory reaction to improve islets of Langerhans engraftment. Curr Opin Organ Transplant. 2011; 16: 620-626. [CrossRef]
- Moberg L, Korsgren O, Nilsson B. Neutrophilic granulocytes are the predominant cell type infiltrating pancreatic islets in contact with ABO-compatible blood. Clin Exp Immunol. 2005; 142: 125-131. [CrossRef]
- Moberg L, Johansson H, Lukinius A, Berne C, Foss A, Källen R, et al. Production of tissue factor by pancreatic islet cells as a trigger of detrimental thrombotic reactions in clinical islet transplantation. The Lancet. 2002; 360: 2039-2045. [CrossRef]
- Sakata N, Chan NK, Chrisler J, Obenaus A, Hathout E. Bone marrow cell co-transplantation with islets improves their vascularization and function. Transplantation. 2010; 89: 686-693. [CrossRef]
- Low G, Hussein N, Owen RJT, Toso C, Patel VH, Bhargava R, et al. Role of imaging in clinical islet transplantation. RadioGraphics. 2010; 30: 353-366. [CrossRef]
- Huang X, Hultgren B, Dybdal N, Stewart TA. Islet expression of interferon-alpha precedes diabetes in both the BB rat and streptozotocin-treated mice. Immunity. 1994; 1: 469-478. [CrossRef]
- 46. Rabinovitch A, Suarez-Pinzon WL, Strynadka K, Schulz R, Lakey JR, Warnock GL, et al. Human pancreatic islet beta-cell destruction by cytokines is independent of nitric oxide production. J Clin Endocrinol Metab. 1994; 79: 1058-1062.
- Jiang Z, Woda BA. Cytokine gene expression in the islets of the diabetic Biobreeding/Worcester rat. J Immunol. 1991; 146: 2990-2994.
- Yamada K, Otabe S, Inada C, Takane N, Nonaka K. Nitric oxide and nitric oxide synthase mRNA induction in mouse islet cells by interferon-γ plus tumor necrosis factor-α. Biochem Bioph Res Commun. 1993; 197: 22-27. [CrossRef]
- Yamada K, Takane N, Otabe S, Inada C, Inoue M, Nonaka K. Pancreatic β-cell–selective production of tumor necrosis factor-α induced by interleukin-1. Diabetes. 1993; 42: 1026-1031. [CrossRef]
- Maedler K, Sergeev P, Ris F, Oberholzer J, Joller-Jemelka HI, Spinas GA, et al. Glucose-induced β cell production of IL-1β contributes to glucotoxicity in human pancreatic islets. J Clin Invest. 2002; 110: 851-860. [CrossRef]
- Böni-Schnetzler M, Thorne J, Parnaud G, Marselli L, Ehses JA, Kerr-Conte J, et al. Increased -nterleukin (IL)-1β messenger ribonucleic acid expression in β-cells of individuals with type 2 diabetes and regulation of IL-1β in human by glucose and autostimulation. J Clin Endocrinol Metab. 2008; 93: 4065-4074. [CrossRef]
- Baker MS, Chen X, Rotramel A, Nelson J, Kaufman DB. Proinflammatory cytokines induce NF-κB-Dependent/NO-independent chemokine gene expression in MIN6 β cells11Supported by National Institutes of Health Grant RO-1 DK52919 and the Juvenile Diabetes Research Foundation. (D.B.K). J Surg Res. 2003; 110: 295-303. [CrossRef]
- Lee I, Wang L, Wells AD, Ye Q, Han R, Dorf ME, et al. Blocking the Monocyte Chemoattractant protein-1/CCR2 chemokine pathway induces permanent survival of islet allografts through a programmed death-1 ligand-1-dependent mechanism. J Immunol. 2003; 171: 6929-6935. [CrossRef]
- Lawrence MC, Naziruddin B, Levy MF, Jackson A, McGlynn K. Calcineurin/nuclear factor of activated T cells and MAPK signaling induce TNF-α gene expression in pancreatic islet endocrine cells. J Biol Chem. 2011; 286: 1025-1036. [CrossRef]
- Yoshimatsu G, Kunnathodi F, Saravanan PB, Shahbazov R, Chang C, Darden CM, et al. Pancreatic beta cell-derived IP-10/CXCL10 isletokine mediates early loss of graft function in islet cell transplantation. Diabetes. 2017; 66: 2857-2867. [CrossRef]
- Torren CR van der, Stuart AAV, Lee D, Meerding J, Velde U van de, Pipeleers D, et al. Serum cytokines as biomarkers in islet cell transplantation for type 1 diabetes. Plos One. 2016; 11: e0146649. [CrossRef]
- Piemonti L, Leone BE, Nano R, Saccani A, Monti P, Maffi P, et al. Human pancreatic islets produce and secrete MCP-1/CCL2: Relevance in human islet transplantation. Diabetes. 2002; 51: 55-65. [CrossRef]
- Bertuzzi F, Marzorati S, Maffi P, Piemonti L, Melzi R, de Taddeo F, et al. Tissue factor and CCL2/monocyte chemoattractant protein-1 released by human islets affect islet engraftment in type 1 diabetic recipients. J Clin Endocrinol Metab. 2004; 89: 5724-5728. [CrossRef]
- Schröppel B, Zhang N, Chen P, Zang W, Chen D, Hudkins KL, et al. Differential expression of chemokines and chemokine receptors in murine islet allografts: The role of CCR2 and CCR5 signaling pathways. JASN. 2004; 15: 1853-1861. [CrossRef]
- Ehrnfelt C, Kumagai-Braesch M, Uzunel M, Holgersson J. Adult porcine islets produce MCP-1 and recruit human monocytes in vitro. Xenotransplantation. 2004; 11: 184-194. [CrossRef]
- Matsuoka N, Itoh T, Watarai H, Sekine-Kondo E, Nagata N, Okamoto K, et al. High-mobility group box 1 is involved in the initial events of early loss of transplanted islets in mice. J Clin Invest. 2010; 120: 735-743. [CrossRef]
- Lee J. Adipose tissue macrophages in the development of obesity-induced inflammation, insulin resistance and type 2 Diabetes. Arch Pharm Res. 2013; 36: 208-222. [CrossRef]
- Fric J, Zelante T, Ricciardi-Castagnoli P. Phagocytosis of particulate antigens – All roads lead to calcineurin/NFAT signaling pathway. Front Immunol. 2014; 4. [CrossRef]
- Schulthess FT, Paroni F, Sauter NS, Shu L, Ribaux P, Haataja L, et al. CXCL10 impairs β cell function and viability in diabetes through TLR4 signaling. Cell Metab. 2009; 9: 125-139. [CrossRef]
- Gerber, Philipp A, Rutter, Guy A. The role of oxidate stress and hypoxia in pancreatic beta-cell dysfunciton in diabetes mellitus. Antioxid Redox Signal. 2017; 26: 501-518. [CrossRef]
- Komatsu H, Kandeel F, Mullen Y. Impact of oxygen on pancreatic islet survival. Pancreas. 2018; 47: 533-543. [CrossRef]
- Pi J, Bai Y, Zhang Q, Wong V, Floering LM, Daniel K, et al. Reactive oxygen species as a signal in glucose-stimulated insulin secretion. Diabetes. 2007; 56: 1783-1791. [CrossRef]
- Leloup C, Tourrel-Cuzin C, Magnan C, Karaca M, Castel J, Carneiro L, et al. Mitochondrial reactive oxygen species are obligatory signals for glucose-induced insulin secretion. Diabetes. 2009; 58: 673-681. [CrossRef]
- Ježek P, Dlasková A, Plecitá-Hlavatá L. Redox homeostasis in pancreatic β cells. Oxid Med Cell Longev. 2012; 2012: 932838. [CrossRef]
- Tiedge M, Lortz S, Drinkgern J, Lenzen S. Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes. 1997; 46: 1733-1742. [CrossRef]
- Newsholme P, Haber EP, Hirabara SM, Rebelato ELO, Procopio J, Morgan D, et al. Diabetes associated cell stress and dysfunction: role of mitochondrial and non-mitochondrial ROS production and activity. J Physiol. 2007; 583: 9-24. [CrossRef]
- Circu ML, Aw TY. Reactive oxygen species, cellular redox systems, and apoptosis. Free Radical Bio Med. 2010; 48: 749-762. [CrossRef]
- Kenneth NS, Rocha S. Regulation of gene expression by hypoxia. Biochem J. 2008; 414: 19-29. [CrossRef]
- Siddiq A, Ayoub IA, Chavez JC, Aminova L, Shah S, LaManna JC, et al. Hypoxia-inducible factor prolyl 4-hydroxylase inhibition a target for neuroprotection in the central nervous system. J Biol Chem. 2005; 280: 41732-41743. [CrossRef]
- Myllyharju J. Prolyl 4-hydroxylases, master regulators of the hypoxia response. Acta Physiologica. 2013; 208: 148-165. [CrossRef]
- Li J, Yuan W, Jiang S, Ye W, Yang H, Shapiro IM, et al. Prolyl-4-hydroxylase domain protein 2 controls NF-κB/p65 transactivation and enhances the catabolic effects of inflammatory cytokines on cells of the nucleus pulposus. J Biol Chem. 2015; 290: 7195-7207. [CrossRef]
- Cummins EP, Berra E, Comerford KM, Ginouves A, Fitzgerald KT, Seeballuck F, et al. Prolyl hydroxylase-1 negatively regulates IκB kinase-β, giving insight into hypoxia-induced NFκB activity. Proc Natl Acad Sci U S A. 2006; 103: 18154-18159. [CrossRef]
- Taylor CT. Interdependent roles for hypoxia inducible factor and nuclear factor-kappaB in hypoxic inflammation. J Physiol (Lond). 2008; 586: 4055-4059. [CrossRef]
- Linn T, Schmitz J, Hauck-Schmalenberger I, Lai Y, Bretzel RG, Brandhorst H, et al. Ischaemia is linked to inflammation and induction of angiogenesis in pancreatic islets. Clin Exp Immunol. 2006; 144: 179-187. [CrossRef]
- Størling J, Binzer J, Andersson AK, Züllig RA, Tonnesen M, Lehmann R, et al. Nitric oxide contributes to cytokine-induced apoptosis in pancreatic beta cells via potentiation of JNK activity and inhibition of Akt. Diabetologia. 2005; 48: 2039-2050. [CrossRef]
- Weaver JR, Holman TR, Imai Y, Jadhav A, Kenyon V, Maloney DJ, et al. Integration of pro-inflammatory cytokines, 12-lipoxygenase and NOX-1 in pancreatic islet beta cell dysfunction. Mol Cell Endocrinol. 2012; 358: 88-95. [CrossRef]
- Brozzi F, Nardelli TR, Lopes M, Millard I, Barthson J, Igoillo-Esteve M, et al. Cytokines induce endoplasmic reticulum stress in human, rat and mouse beta cells via different mechanisms. Diabetologia. 2015; 58: 2307-2316. [CrossRef]
- Åkerfeldt MC, Howes J, Chan JY, Stevens VA, Boubenna N, McGuire HM, et al. Cytokine-induced β-cell death is independent of endoplasmic reticulum stress signaling. Diabetes. 2008; 57: 3034-3044. [CrossRef]
- Miani M, Barthson J, Colli ML, Brozzi F, Cnop M, Eizirik DL. Endoplasmic reticulum stress sensitizes pancreatic beta cells to interleukin-1β-induced apoptosis via Bim/A1 imbalance. Cell Death Dis. 2013; 4: e701. [CrossRef]
- Weichhart T, Costantino G, Poglitsch M, Rosner M, Zeyda M, Stuhlmeier KM, et al. The TSC-mTOR signaling pathway regulates the innate inflammatory response. Immunity. 2008; 29: 565-577. [CrossRef]
- Schmitz F, Heit A, Dreher S, Eisenächer K, Mages J, Haas T, et al. Mammalian target of rapamycin (mTOR) orchestrates the defense program of innate immune cells. Eur J Immunol. 2008; 38: 2981-2992. [CrossRef]
- Kang YJ, Kusler B, Otsuka M, Hughes M, Suzuki N, Suzuki S, et al. Calcineurin negatively regulates TLR-mediated activation pathways. J Immunol. 2007; 179: 4598-4607. [CrossRef]
- Jennings C, Kusler B, Jones PP. Calcineurin inactivation leads to decreased responsiveness to LPS in macrophages and dendritic cells and protects against LPS-induced toxicity in vivo. Innate Immun. 2009; 15: 109-120. [CrossRef]
- Fraenkel M, Ketzinel-Gilad M, Ariav Y, Pappo O, Karaca M, Castel J, et al. mTOR inhibition by rapamycin prevents β-cell adaptation to hyperglycemia and exacerbates the metabolic state in type 2 diabetes. Diabetes. 2008; 57: 945-957. [CrossRef]
- Velde SV de, Hogan MF, Montminy M. mTOR links incretin signaling to HIF induction in pancreatic beta cells. PNAS. 2011; 108: 16876-16882. [CrossRef]
- Sinagoga KL, Stone WJ, Schiesser JV, Schweitzer JI, Sampson L, Zheng Y, et al. Distinct roles for the mTOR pathway in postnatal morphogenesis, maturation and function of pancreatic islets. Development. 2017; 144: 2402-2414. [CrossRef]
- Lombardi A, Gambardella J, Du X-L, Sorriento D, Mauro M, Iaccarino G, et al. Sirolimus induces depletion of intracellular calcium stores and mitochondrial dysfunction in pancreatic beta cells. Sci Rep. 2017; 7: 15823. [CrossRef]
- Zanoni I, Ostuni R, Capuano G, Collini M, Caccia M, Ronchi AE, et al. CD14 regulates the dendritic cell life cycle after LPS exposure through NFAT activation. Nature. 2009; 460: 264-268. [CrossRef]
- Shin DS, Jordan A, Basu S, Thomas RM, Bandyopadhyay S, Zoeten EF de, et al. Regulatory T cells suppress CD4+ T cells through NFAT‐dependent transcriptional mechanisms. EMBO Rep. 2014; 15: 991-999. [CrossRef]
- Ferreira GB, Vanherwegen AS, Eelen G, Gutiérrez ACF, Van Lommel L, Marchal K, et al. Vitamin D3 induces tolerance in human dendritic cells by activation of intracellular metabolic pathways. Cell Rep. 2015; 10: 711-725. [CrossRef]
- Naziruddin B, Kanak MA, Chang CA, Takita M, Lawrence MC, Dennison AR, et al. Improved outcomes of islet autotransplant after total pancreatectomy by combined blockade of IL-1β and TNFα. Am J Transplant. 2018; 18: 2322-2329. [CrossRef]
- Tanaka S, Nishida Y, Aida K, Maruyama T, Shimada A, Suzuki M, et al. Enterovirus infection, CXC chemokine ligand 10 (CXCL10) and CXCR3 circuit: a mechanism of accelerated beta-cell failure in fulminant type 1 diabetes. Diabetes. 2009; 58: 2285-2291. [CrossRef]
- Roep BO, Kleijwegt FS, Halteren AGSV, Bonato V, Boggi U, Vendrame F, et al. Islet inflammation and CXCL10 in recent-onset type 1 diabetes. Clin Exp Immunol. 2010; 159: 338-343. [CrossRef]
- Bender C, Christen S, Scholich K, Bayer M, Pfeilschifter JM, Hintermann E, et al. Islet-expressed CXCL10 promotes autoimmune destruction of islet isografts in mice with type 1 diabetes. Diabetes. 2017; 66: 113-126. [CrossRef]
- Lasch S, Müller P, Bayer M, Pfeilschifter JM, Luster AD, Hintermann E, et al. Anti-CD3/anti-CXCL10 antibody combination therapy induces a persistent remission of type 1 diabetes in two mouse models. Diabetes. 2015; 64: 4198-4211. [CrossRef]
- Melzi R, Mercalli A, Sordi V, Cantarelli E, Nano R, Maffi P, et al. Role of CCL2/MCP-1 in islet transplantation. Cell Transplant. 2010; 19: 1031-1046. [CrossRef]
- Ozbay LA, Møller N, Juhl C, Bjerre M, Carstens J, Rungby J, et al. The impact of calcineurin inhibitors on insulin sensitivity and insulin secretion: a randomized crossover trial in uraemic patients. Diabet Med. 2012; 29: e440-e444. [CrossRef]
- Kloster-Jensen K, Sahraoui A, Vethe NT, Korsgren O, Bergan S, Foss A, et al. Treatment with tacrolimus and sirolimus reveals no additional adverse effects on human islets in vitro compared to each drug alone but they are reduced by adding glucocorticoids. J Diabetes Res. 2016; 2016: 4196460. [CrossRef]
- Øzbay LA, Møller N, Juhl C, Bjerre M, Carstens J, Rungby J, et al. Calcineurin inhibitors acutely improve insulin sensitivity without affecting insulin secretion in healthy human volunteers. Br J Clin Pharmacol. 2012; 73: 536-545. [CrossRef]
- Ranta F, Avram D, Berchtold S, Düfer M, Drews G, Lang F, et al. Dexamethasone induces cell death in insulin-secreting cells, an effect reversed by exendin-4. Diabetes. 2006; 55: 1380-1390. [CrossRef]
- Balibrea del Castillo JM, García-Martín MC, Arias-Díaz J, Giné E, Vara E, Balibrea Cantero JL. Antiapoptotic effect of tacrolimus on cytokine-challenged human islets. 2009; 18: 1237-1246.
- Lawrence MC, McGlynn K, Park B-H, Cobb MH. ERK1/2-dependent activation of transcription factors required for acute and chronic effects of glucose on the insulin gene promoter. J Biol Chem. 2005; 280: 26751-26759. [CrossRef]
- Paraskevas S, Aikin R, Maysinger D, Lakey JRT, Cavanagh TJ, Agapitos D, et al. Modulation of JNK and p38 stress activated protein kinases in isolated islets of langerhans. Ann Surg. 2001; 233: 124-133. [CrossRef]
- Matsuda T, Omori K, Vuong T, Pascual M, Valiente L, Ferreri K, et al. Inhibition of p38 pathway suppresses human islet production of pro-inflammatory cytokines and improves islet graft function. Am J Transplant. 2005; 5: 484-493. [CrossRef]
- Noguchi H, Nakai Y, Ueda M, Masui Y, Futaki S, Kobayashi N, et al. Activation of c-Jun NH2-terminal kinase (JNK) pathway during islet transplantation and prevention of islet graft loss by intraportal injection of JNK inhibitor. Diabetologia. 2007; 50: 612-619. [CrossRef]
- Fornoni A, Pileggi A, Molano RD, Sanabria NY, Tejada T, Gonzalez-Quintana J, et al. Inhibition of c-jun N terminal kinase (JNK) improves functional beta cell mass in human islets and leads to AKT and glycogen synthase kinase-3 (GSK-3) phosphorylation. Diabetologia. 2008; 51: 298-308. [CrossRef]
- 112. Noguchi H, Miyagi-Shiohira C, Nakashima Y, Ebi N, Hamada E, Tamaki Y, et al. Modified cell-permeable JNK inhibitors efficiently prevents islet apoptosis and improves the outcome of islet transplantation. Sci Rep. 2018; 8. [CrossRef]
- Chang CA, Akinbobuyi B, Quintana JM, Yoshimatsu G, Naziruddin B, Kane RR. Ex-vivo generation of drug-eluting islets improves transplant outcomes by inhibiting TLR4-Mediated NFkB upregulation. Biomaterials. 2018; 159: 13-24. [CrossRef]
- Tipping PG. Toll-Like Receptors: The Interface between Innate and Adaptive Immunity. JASN. 2006; 17: 1769-1771. [CrossRef]
- Krüger B, Yin N, Zhang N, Yadav A, Coward W, Lal G, et al. Islet-expressed TLR2 and TLR4 sense injury and mediate early graft failure after transplantation. Eur J Immunol. 2010; 40: 2914-2924. [CrossRef]
- 116. Vazquez-Torres A, Vallance BA, Bergman MA, Finlay BB, Cookson BT, Jones-Carson J, et al. Toll-like receptor 4 dependence of innate and adaptive immunity to salmonella: Importance of the kupffer cell network. J Immunol. 2004; 172: 6202-6208. [CrossRef]
- Loures FV, Pina A, Felonato M, Feriotti C, de Araújo EF, Calich VLG. MyD88 signaling is required for efficient innate and adaptive immune responses to paracoccidioides brasiliensis infection. Infect Immun. 2011; 79: 2470-2480. [CrossRef]
- Oliveira A-C, Alencar BC de, Tzelepis F, Klezewsky W, Silva RN da, Neves FS, et al. Impaired innate immunity in Tlr4−/− mice but preserved CD8+ T cell responses against trypanosoma cruzi in Tlr4-, Tlr2-, Tlr9- or Myd88-deficient mice. Plos Pathog. 2010; 6: e1000870. [CrossRef]
- Schnare M, Barton GM, Holt AC, Takeda K, Akira S, Medzhitov R. Toll-like receptors control activation of adaptive immune responses. Nat Immunol. 2001; 2: 947-950. [CrossRef]
- Johansson H, Lukinius A, Moberg L, Lundgren T, Berne C, Foss A, et al. Tissue factor produced by the endocrine cells of the islets of langerhans is associated with a negative outcome of clinical islet transplantation. Diabetes. 2005; 54: 1755-1762. [CrossRef]
- Ozmen L, Ekdahl KN, Elgue G, Larsson R, Korsgren O, Nilsson B. Inhibition of thrombin abrogates the instant blood-mediated inflammatory reaction triggered by isolated human islets: possible application of the thrombin inhibitor melagatran in clinical islet transplantation. Diabetes. 2002; 51: 1779-1784. [CrossRef]
- Koulmanda M, Bhasin M, Fan Z, Hanidziar D, Goel N, Putheti P, et al. Alpha 1-antitrypsin reduces inflammation and enhances mouse pancreatic islet transplant survival. Proc Natl Acad Sci U S A. 2012; 109: 15443-15448. [CrossRef]
- Wang J, Sun Z, Gou W, Adams DB, Cui W, Morgan KA, et al. α-1 antitrypsin enhances islet engraftment by suppression of instant blood-mediated inflammatory reaction. Diabetes. 2017; 66: 970-980. [CrossRef]


